Changing trends in cholecystectomy approaches amid the COVID-19 pandemic: From laparoscopy to laparotomy
Cholecystectomy trends during COVID-19
Authors
Abstract
Aim The COVID-19 pandemic profoundly affected surgical services worldwide, resulting in delays in care, modifications of surgical practice, and altered perioperative outcomes. This study aimed to evaluate the impact of the pandemic on cholecystectomy by comparing demographic, clinical, and perioperative variables between the pre-pandemic and pandemic periods.
Materials and Methods A retrospective, single-center analysis was performed on patients who underwent cholecystectomy between January 2018 and March 2022. Two groups were defined: pre-pandemic (January 2018–February 2020) and pandemic (March 2020–March 2022). Demographic data, surgical approach, operative time, and length of hospital stay were evaluated. Statistical analyses included the Kolmogorov–Smirnov test, independent samples t-test, and Chi-square test, with significance set at p<0.05.
Results A total of 2,760 patients were analyzed, with 1,516 in the pre-pandemic group and 1,244 in the pandemic group. Patients in the pandemic group were older on average (50.0 ± 14.9 vs. 48.3 ± 13.9 years, p < 0.01). Open cholecystectomy increased significantly (6.5% vs. 3.0%, p < 0.01), while laparoscopic procedures decreased. Operative time was longer (75.1 ± 36.4 vs. 50.7 ± 13.4 minutes, p < 0.01), and hospital stay was slightly prolonged (2.35 ± 2.73 vs. 2.17 ± 1.63 days, p < 0.05).
Discussion The COVID-19 pandemic significantly altered cholecystectomy practice, with older patient profiles, increased open procedures, longer operative times, and extended hospitalization. These findings highlight the vulnerability of surgical services during global health crises and emphasize the need for adaptive perioperative strategies, maintenance of minimally invasive access, and organizational preparedness to safeguard surgical outcomes in future pandemics.
Keywords
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, first reported in Wuhan, China, in December 2019, rapidly evolved into a global health crisis and placed an extraordinary strain on healthcare systems worldwide. On March 11, 2020, the World Health Organization (WHO) officially declared COVID-19 a pandemic, prompting radical restructuring of healthcare delivery and prioritization of resources toward infection control and critical care [1]. Surgical services were among the most affected, with widespread postponement of elective procedures and a shift toward emergency interventions [2]. Operating rooms were reorganized through stringent infection-control protocols, enhanced use of personal protective equipment (PPE), and modified perioperative pathways to minimize viral transmission [3, 4].
Gallbladder diseases, particularly cholelithiasis, affect approximately 10–15% of the adult population and represent a major healthcare burden [5]. Cholecystectomy is the definitive treatment for symptomatic gallstones and related complications [6]. Laparoscopic cholecystectomy has long been the gold standard due to advantages such as shorter hospitalization, reduced postoperative pain, faster recovery, and lower wound complication rates [7]. However, during the pandemic, concerns about potential aerosolization of viral particles during laparoscopy led many centers to restrict its use, contributing to a relative increase in open cholecystectomy [8].
These practice changes were compounded by delays in surgical timing, resulting in patients presenting at an older age or with more advanced disease. The international ChoCO-W study reported that COVID-19- positive patients had significantly higher rates of open cholecystectomy and nearly double the incidence of gangrenous cholecystitis, along with longer hospital stays and increased complication rates [9]. Workforce shortages, extended preoperative preparation, and logistic constraints were also shown to adversely affect surgical workflow and patient outcomes worldwide [10].
The present study aimed to evaluate the impact of the COVID-19 pandemic on cholecystectomy practice by comparing cases performed before and during the pandemic with respect to demographic characteristics, surgical approach, operative time, and length of hospital stay. By providing a large, single-center analysis, this study seeks to contribute evidence to guide surgical planning and resource allocation in future global health crises.
Materials and Methods
This was a single-center, retrospective, comparative study. Data from all consecutive patients who underwent cholecystectomy at our institution between January 2018 and March 2022 were reviewed. Based on the date of surgery, patients were divided into two cohorts: pre-pandemic (January 2018–February 2020) and pandemic (March 2020–March 2022). COVID-19 negativity was confirmed preoperatively by polymerase chain reaction (PCR) testing. Patients with incomplete medical records, those who underwent concomitant major surgical procedures, or those with malignant biliary disease were excluded.
Demographic variables (age, sex), surgical approach (laparoscopic or open cholecystectomy), operative time (minutes), and length of hospital stay (days) were retrieved from the electronic medical record system.
Statistical Analysis
All statistical analyses were performed using SPSS for Windows, version 22.0 (IBM Corp., Armonk, NY, USA). The normality of continuous variables was assessed using the Kolmogorov–Smirnov test. An independent samples t-test was applied for continuous variables, and the Chi- square test was used for categorical variables. Results were expressed as mean ± standard deviation or percentage (%). A p-value <0.05 was considered statistically significant.
Ethical Approval
This study was approved by the Ethics Committee of Malatya Turgut Özal University (Date: 2025-02-24, No: E-30785963-020-287128).
Results
A total of 2,760 patients were included in the study, of whom 1,516 (54.9%) underwent cholecystectomy in the pre-pandemic period and 1,244 (45.1%) during the pandemic. The mean age of patients was significantly higher in the pandemic cohort compared with the pre- pandemic cohort (50.03 ± 14.89 vs. 48.29 ± 13.87 years; t = –3.17; p < 0.01). There was no statistically significant difference between the groups regarding gender distribution (p = 0.06). In the pre-pandemic cohort, males accounted for 21.7% (n = 329) and females 78.3% (n = 1,187), whereas during the pandemic, males accounted for 24.8% (n = 308) and females 75.2% (n = 936).
Comparison of surgical approaches revealed a significant increase in the rate of open cholecystectomy during the pandemic, with a corresponding decrease in laparoscopic procedures. In the pre- pandemic period, the rate of open cholecystectomy was 2.97% (n = 45), and laparoscopic cholecystectomy was 97.03% (n = 1,471). In contrast, during the pandemic, the rate of open procedures increased to 6.51% (n = 81), while laparoscopic procedures decreased to 93.49% (n = 1,163) (χ² = 19.69; p < 0.01) (Table 1).
The mean length of hospital stay was significantly longer during the pandemic compared with the pre-pandemic period (2.35 ± 2.73 vs. 2.17 ± 1.63 days; t = –2.08; p < 0.05). Operative time also showed a marked increase in the pandemic cohort, rising from 50.70 ± 13.40 minutes before the pandemic to 75.06 ± 36.44 minutes during the pandemic (t = –24.12; p < 0.01) (Table 2).
Discussion
The COVID-19 pandemic has profoundly influenced surgical practice worldwide, leading to delays in presentation, changes in operative strategies, and altered perioperative outcomes [11]. Consistent with these global trends, our analysis demonstrated that patients undergoing cholecystectomy during the pandemic were significantly older at the time of surgery, reflecting delayed hospital admissions and more advanced disease severity reported in recent studies [12]. We also observed a higher rate of open cholecystectomy during the pandemic, in agreement with the ChoCO-W international cohort, which documented increased open procedures and more complicated gallbladder pathology in COVID-19-positive patients [13]. In addition, both operative time and length of hospital stay were significantly prolonged, likely reflecting the impact of strict infection-control protocols and healthcare resource constraints described in prior reports [14].
During the pandemic, the proportion of open cholecystectomies in our cohort rose significantly to 6.5%, a finding consistent with observations from other centers worldwide. Several mechanisms may explain this trend. Case-mix changes and staff shortages have been linked to poorer outcomes and higher open conversion rates during the pandemic [15]. More advanced presentations of acute cholecystitis also contributed to increased case complexity, as reported in the University of Szeged series, which demonstrated higher rates of perforation and percutaneous interventions [16]. Similarly, a large multicenter Italian study found that the management of acute calculous cholecystitis during the pandemic was characterized by delayed treatment and more severe clinical presentations, factors likely associated with the greater reliance on open procedures [17].
The longer operative times observed in our study may be explained by several pandemic-related factors, including mandatory use of enhanced personal protective equipment, strict infection-control measures, extended preoperative workflows, and a higher proportion of patients presenting with advanced disease. Comparable findings have been reported in a recent multicenter cohort study from Europe, which demonstrated that urgent gastrointestinal surgeries performed during the COVID-19 pandemic were associated with longer operative durations and poorer perioperative outcomes compared with pre- pandemic cases [18]. These observations reinforce the notion that systemic constraints and heightened safety protocols introduced during the pandemic substantially contributed to delays in surgical care.
The prolongation of hospital stay observed in our study is consistent with the growing body of evidence describing the impact of the COVID-19 pandemic on perioperative care. Under normal conditions, laparoscopic cholecystectomy is associated with earlier discharge; however, during the pandemic, mandatory isolation protocols, extended turnaround times for COVID-19 testing, and a more cautious postoperative approach collectively contributed to longer admissions. These findings align with Italian data, where Bressan et al. demonstrated that prolonged preoperative waiting times in urgent laparoscopic cholecystectomy were directly associated with significantly longer hospital stays [19]. Their analysis highlighted that delays in surgical intervention—whether due to systemic overload or infection-control precautions—substantially increased the duration of inpatient care. Taken together, these results emphasize that minimizing delays to surgery and streamlining perioperative protocols are critical to reducing hospital stay in future pandemic scenarios.
The higher mean patient age observed during the pandemic in our cohort may be explained by behavioral changes in healthcare- seeking patterns. Elderly individuals, in particular, were likely to delay seeking medical care due to fear of contracting COVID-19, resulting in more advanced or complicated disease at the time of admission. This interpretation is supported by a retrospective study reporting that during the COVID-19 outbreak, patients with acute cholecystitis presented significantly later after symptom onset and exhibited more severe clinical manifestations compared with the pre-pandemic period [20]. These findings provide valuable context for our results, suggesting that both behavioral and clinical factors contributed to the older age distribution observed among patients undergoing cholecystectomy during the pandemic.
Tables
Table 1. Demographic characteristics and surgical approach of patients undergoing cholecystectomy before and during the COVID-19 pandemic
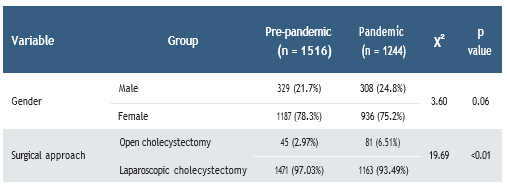
χ²: Chi-square test.
Table 2. Comparison of age, operative time, and length of hospital stay between the pre-pandemic and pandemic groups
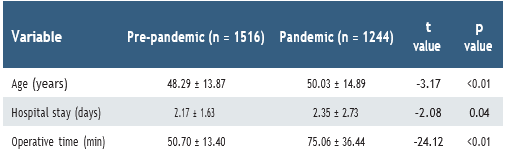
Values are presented as mean ± standard deviation. An independent samples t-test was used.
Limitations
The strengths of our study include the relatively large sample size and the direct comparison of pre-pandemic and pandemic periods within a single institution, which allowed for a consistent analysis of demographic and perioperative variables. Nevertheless, several limitations should be acknowledged. First, the retrospective design may have introduced inherent biases related to data collection and interpretation. Second, as this was a single-center experience, the findings may not be fully generalizable to other institutions or healthcare systems with different resources and pandemic responses. Third, we did not perform multivariate analyses, which limits the ability to determine independent risk factors and adjust for potential confounders. Finally, the absence of a detailed assessment regarding disease severity and postoperative complication rates represents an additional limitation that may restrict the comprehensiveness of our conclusions.
Conclusion
The COVID-19 pandemic significantly altered the practice of cholecystectomy, with patients presenting at an older age, a clear increase in open procedures, longer operative times, and extended hospital stays. These changes likely reflect not only modifications in surgical decision-making but also the systemic constraints, logistical challenges, and behavioral factors imposed by the pandemic. Our results, consistent with international experiences, highlight the vulnerability of surgical services during global health crises and demonstrate the necessity of resilient perioperative strategies. To safeguard essential surgical care in future pandemics or similar emergencies, adaptive and evidence-based algorithms should be prioritized. Ensuring timely access to surgery, maintaining the availability of minimally invasive techniques, and optimizing perioperative workflows are critical steps in reducing delays and improving outcomes. In addition, organizational preparedness, workforce flexibility, and efficient resource allocation will be key to mitigating the adverse consequences of systemic disruptions on surgical practice and patient safety.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Bourgeois C, Oyaert L, Van de Velde M, et al. Pain management after laparoscopic cholecystectomy: a systematic review and procedure-specific postoperative pain management (PROSPECT) recommendations. Eur J Anaesthesiol. 2024;41(11):841-55.
-
COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107(11):1440-49.
-
Al-Jabir A, Kerwan A, Nicola M, et al. Impact of the Coronavirus (COVID-19) pandemic on surgical practice - Part 1. Int J Surg. 2020;79:168-79.
-
Singhal R, Dickerson L, Sakran N, et al. Safe surgery during the COVID-19 pandemic. Curr Obes Rep. 2022;11(3):203-14.
-
Shabanzadeh DM. Incidence of gallstone disease and complications. Curr Opin Gastroenterol. 2018;34(2):81-9.
-
Pisano M, Allievi N, Gurusamy K, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020;15(1):61.
-
Wu H, Liao B, Cao T, et al. Comparison of the safety profile, conversion rate and hospitalization duration between early and delayed laparoscopic cholecystectomy for acute cholecystitis: a systematic review and meta-analysis. Front Med (Lausanne). 2023;10:1185482.
-
Vigneswaran Y, Prachand VN, Posner MC, Matthews JB, Hussain M. What is the appropriate use of laparoscopy over open procedures in the current COVID-19 climate? J Gastrointest Surg. 2020;24(7):1686-91.
-
De Simone B, Abu-Zidan FM, Chouillard E, et al. The ChoCO-W prospective observational global study: does COVID-19 increase gangrenous cholecystitis?. World J Emerg Surg. 2022;17(1):61.
-
Kamil AM, Davey MG, Marzouk F, et al. The impact of COVID-19 on emergency surgical presentations in a university teaching hospital. Ir J Med Sci. 2022;191(3):1059-65.
-
Sakong D, Choe MSP, Nho WY, Park CW. Impact of COVID-19 outbreak on acute gallbladder disease in the emergency department. Clin Exp Emerg Med. 2023;10(1):84-91.
-
Fouad MMB, Rezk SSS, Saber AT, Khalifa A, Ibraheim P, Ibraheim SMN. Effect of the COVID-19 pandemic on the management of acute cholecystitis and assessment of the crisis approach: a multicenter experience in Egypt. Asian J Endosc Surg. 2022;15(1):128-36.
-
Cochrun SL Jr, Finnegan T, Kennedy GE, Garland M, Grams JM, Parmar AD. A retrospective single-institution review of the impact of COVID-19 on severity of biliary disease. Am J Surg. 2023;225(2):352-6.
-
Demetriou G, Wanigasooriya K, Elmaradny A, et al. The impact of the COVID-19 pandemic on elective laparoscopic cholecystectomy: a retrospective cohort study. Front Surg. 2022;9:990533.
-
Abdelsamad A, Ibrahim E, Elsheikh A, et al. Worse cholecystectomy outcomes during the COVID-19 pandemic: were staff shortages or a change in patient case-mix the culprit? Surg Endosc. 2024;38(12):7389-98.
-
Tóth I, Ábrahám S, Karamya Z, et al. Multidisciplinary management of acute cholecystitis during the COVID-19 pandemic. Sci Rep. 2023;13(1):16257.
-
Stavridis K, Liosis I, Konstantinidis MK, Kondylis G, Ioannidis A. COVID-19 and acute cholecystitis management: a systematic review of current literature. Front Surg. 2022;9:871685.
-
Gouel-Chéron A, Sallah K, Sawadogo S, Dupont A, Montravers P. Impact of COVID-19 on urgent gastrointestinal surgery outcomes: increased mortality in 2020. World J Emerg Surg. 2025;20(1):23.
-
Bressan L, Cimino MM, Vaccari F, et al. Preoperative waiting time affects the length of stay of patients treated via laparoscopic cholecystectomy in an acute care surgical setting. J Clin Med. 2024;13(23):7263.
-
Hershkovitz Y, Zmora O, Nativ H, Ashkenazi I, Hammerschlag J, Jeroukhimov I. Clinical presentation of acute cholecystitis during the COVID-19 outbreak. Isr Med Assoc J. 2022;24(5):306-9.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Malatya Turgut Özal University (Date: 2025-02-24, No: E-30785963-020-287128)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Bahadır Öndeş, Osman Gökhan Gökdere, Fatih Gönültaş. Changing trends in cholecystectomy approaches amid the COVID-19 pandemic: From laparoscopy to laparotomy. Eu Clin Anal Med 2025;13(Suppl 1):S11-14
Publication History
- Received:
- September 20, 2025
- Accepted:
- October 20, 2025
- Published Online:
- October 24, 2025
- Printed:
- October 25, 2025
