Surgical approach and clinical outcomes in giant hydatid cyst cases
Management of giant hydatid cysts
Authors
Abstract
Aim Giant hydatid cysts pose significant surgical challenges due to their large size and are associated with an increased risk of complications. This study aimed to retrospectively evaluate the clinical outcomes and complication profiles of open and laparoscopic surgical approaches in patients with hydatid cysts ≥100 mm, and to compare the differences between these approaches.
Materials and Methods Between September 2020 and May 2025, 32 patients underwent surgery for hydatid cysts in our clinic. Of these, 13 patients with radiologically measured cyst diameters ≥100 mm were included. Demographic data, surgical methods, postoperative complications, and hospital stay durations were analyzed.
Results The mean age of the giant cyst group was 48.5 years (range: 18–76), including 7 males and 6 females. Abdominal pain was the most common presenting symptom. Open surgery was performed in 8 patients (61.5 %) and laparoscopic surgery in 5 patients (38.5 %). Postoperative complications occurred in 3 patients (23.1 %): one bile fistula in the open group and two cases of atelectasis in the laparoscopic group. The mean postoperative hospital stay was 6.7 days (median: 6 days). No mortality was observed.
Discussion Although giant hydatid cysts present considerable technical challenges, laparoscopic surgery can be safely performed in selected patients. Open surgery remains reliable in complicated cases, while the laparoscopic approach may be considered as an alternative option in the management of giant hydatid cysts.
Keywords
Introduction
Cystic echinococcosis (CE), caused by Echinococcus granulosus sensu lato, remains a major global public health concern [1]. This zoonotic parasitic disease is especially prevalent in regions with dense sheep and dog populations, including the Mediterranean, the Middle East, South America, Africa, and Central Asia [2]. According to the World Health Organization, the annual incidence in endemic areas has been reported to range between 1 and 200 per 100,000 population [3]. Beyond its clinical impact, CE represents a substantial socioeconomic burden because of its chronic course, high morbidity, recurrence potential, and considerable treatment costs [4].
Hydatid cysts are most commonly localized in the liver, accounting for nearly two-thirds of cases, followed by the lungs, which represent the second most frequent site [5]. Less frequently, the spleen, kidneys, brain, and bones may also be involved. The clinical presentation is highly variable and depends on the cyst size, anatomical location, and presence of complications, ranging from asymptomatic disease to life- threatening emergencies [6].
In the literature, hydatid cysts measuring ≥10 cm are widely regarded as “giant cysts,” and their diagnosis and management are considered more complex compared to smaller lesions [7]. Studies have shown that giant cysts are frequently associated with complications such as compression of adjacent organs (gall bladder, stomach, colon…) and communication with biliary structures [8]. Surgical removal of these large cysts also tends to be more technically demanding, often resulting in longer operative times, a higher rate of postoperative morbidity, and extended hospital stays.
Hydatid cysts larger than 10 cm are generally defined in the literature as “giant cysts,” and their diagnostic and therapeutic management is considerably more complex than that of smaller lesions [9]. Increased cyst size has been shown to correlate with higher rates of postoperative complications, particularly when rupture or communication with adjacent structures occurs [10]. In hepatic hydatid disease, retrospective analyses comparing open and laparoscopic surgery indicate that laparoscopy can provide shorter hospital stays and similar morbidity rates in selected cases, although its role in giant cysts remains uncertain [11].
In this study, we retrospectively evaluated the clinical characteristics, surgical techniques, complications, and outcomes of patients who underwent surgery for giant hydatid cysts in our center, intending to contribute further evidence to the literature.
Materials and Methods
Study Design and Patient Selection
This single-center study was designed retrospectively. A total of 32 patients who underwent surgery for hydatid cyst disease between September 2020 and May 2025 at our institution were evaluated. Patients with a radiologically confirmed cyst diameter ≥100 mm, as determined by ultrasonography and/or computed tomography, were defined as having “giant hydatid cysts” and were included in the study cohort.
Data Collection
Medical records and electronic hospital databases were reviewed to collect demographic data (age, sex), presenting symptoms, radiological findings, and laboratory parameters, including C-reactive protein (CRP), hemoglobin (Hb), white blood cell count (WBC), and liver function tests. Cyst localization and size were recorded. Operative details such as surgical procedure (cystectomy, pericystectomy, etc.), surgical approach (open or laparoscopic), intraoperative findings, preoperative and postoperative complications, additional interventions, and postoperative length of hospital stay were analyzed.
Surgical Technique
The choice of surgical method was based on the patient’s overall condition, cyst localization, size, and intraoperative findings. Open procedures were performed through a median or subcostal incision, whereas laparoscopic procedures were carried out using standard trocar placement. In all cases, cyst contents were aspirated, followed by inactivation with a scolicidal agent. Depending on intraoperative assessment, either cystectomy or pericystectomy was performed when appropriate.
Statistical Analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 27.0 (IBM Corp., Armonk, NY, USA). Only descriptive statistics were used, given the retrospective design and limited sample size. Continuous variables were expressed as mean ± standard deviation (SD) or median (minimum–maximum), while categorical variables were presented as frequencies and percentages. No comparative statistical tests were applied.
Informed Consent
Written informed consent had been obtained from all patients prior to surgery.
Ethical Approval
The study was approved by the Ethics Committee of Malatya Turgut Özal University (Date: 2025-09-16, No: E-30785963-020-331201).
Results
Among the 32 patients who underwent surgery for hydatid cyst disease, 13 (40.6 %) had a radiologically confirmed cyst diameter ≥100 mm and were classified as having giant hydatid cysts. The mean age of this group was 48.5 years (range: 18–76), and the cohort consisted of 7 males (53.8 %) and 6 females (46.2 %). The most common presenting symptom was abdominal pain(Table 1). Cystectomy was the most frequently performed surgical procedure. Of the patients with giant cysts, 8 (61.5 %) underwent open surgery and 5 (38.5 %) underwent laparoscopic surgery. Open surgery was more often chosen for multiple, complicated, or deeply located cysts, whereas laparoscopy was preferentially applied in patients with single, accessible cysts without complications.
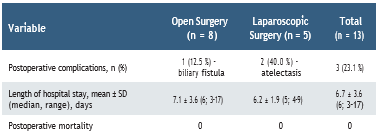
In the postoperative period, complications were observed in 3 patients (23.1 %). In the open surgery group, one patient (12.5 %) developed a biliary fistula, while in the laparoscopic group, 2 patients (40.0 %) experienced atelectasis. No preoperative complications or postoperative mortality were recorded in the study cohort.
The mean postoperative length of hospital stay in the giant cyst group was 6.7 days, with a median of 6 days. Hospitalization was notably prolonged in patients who developed complications, particularly in the case of biliary fistula(Table 2).
Discussion
Open surgery has long been accepted as the gold standard for hydatid cyst surgery due to its advantages in large, multiple, or complicated cases, where the surgeon requires a wide operative field and excellent intraoperative control. However, with the rise of minimally invasive techniques, laparoscopic hydatid cyst surgery has become increasingly utilized, especially in carefully selected patients, and has been reported as a safe alternative in terms of morbidity and recovery [12]. A recent comprehensive comparison among PAIR, laparoscopic, and open surgery modalities demonstrated that cyst size, cyst localization, and preoperative biliary communication are independent predictors of postoperative complication risk, underscoring that open surgery remains preferable in complex cysts [13]. Nevertheless, the feasibility and safety of laparoscopic management in giant hydatid cysts (>10 cm) remain controversial, particularly considering technical challenges, potential cyst rupture, and involvement of biliary structures [14].
In this study, surgical approaches were compared in patients with giant hydatid cysts, defined radiologically as those measuring≥100 mm. The mean age of patients undergoing open surgery was 40.6 years, whereas the mean age in the laparoscopic group was 57.7 years. Although this numerical difference was observed, our findings suggest that the choice of surgical method was not primarily age-related but rather depended on cyst complexity and localisation. Open surgery was more frequently performed in complicated cases, while laparoscopic surgery was preferentially applied when cysts were located in accessible and suitable sites. Similar observations have been reported in recent comparative studies, emphasizing that cyst localization and morphological characteristics, rather than patient age, are the main determinants of whether a laparoscopic or open approach is selected [15].
When complication profiles were evaluated, biliary fistula was observed in the open surgery group, whereas atelectasis was detected in the laparoscopic group. Biliary fistula is a well-known complication of hydatid cyst surgery, particularly in large cysts located near the hepatic hilum. In contrast, the atelectasis observed in the laparoscopic group is likely related more to anesthesia and postoperative pulmonary care than to the surgical technique itself. Although the complication rate was higher in the laparoscopic group (33.3%) compared with the open surgery group (14.3%), it is important that none of these complications resulted in mortality and that most resolved with conservative management. Similar findings have been reported in recent series, in which biliary fistulas were among the most frequent postoperative complications after hepatic hydatid disease surgery, and pulmonary atelectasis has also been described postoperatively—especially when larger or giant cysts are involved [16, 17].
In our analysis, the mean length of hospital stay was 7.1 days in the open surgery group and 6.2 days in the laparoscopic group. Median values further demonstrated the advantage of laparoscopy in reducing hospitalization. This finding is in line with a recent meta-analysis, which reported that laparoscopic management of hepatic hydatid cysts is consistently associated with shorter hospital stays compared to open surgery, without an increase in morbidity or complication rates [18]. In our series, this trend was also observed; however, hospitalization was prolonged in patients who developed complications, particularly in cases complicated by biliary fistula.
In the current literature, laparoscopic surgery is being reported with increasing frequency in the management of giant hydatid cysts; nevertheless, it remains controversial because of technical difficulties and the potential risk of cyst rupture with peritoneal dissemination. Recent reviews emphasize that laparoscopy should be limited to carefully selected patients with favorable cyst localisation and anatomy [19]. Open surgery, on the other hand, is generally associated with longer hospital stays and a greater perioperative burden, whereas laparoscopic procedures tend to reduce hospitalization in appropriately chosen cases. Our findings are in line with the results of Bayrak and Altıntas, who demonstrated in their single-center experience that laparoscopic surgery could be safely performed in selected patients and was associated with shorter length of stay compared with open procedures [20]. Consistent with these observations, our series further suggests that laparoscopic surgery may be feasible in selected giant cysts, although the risk and type of complications must always be considered when determining the operative approach.
Tables
Table 1. Demographic and clinical characteristics of patients with giant hydatid cysts
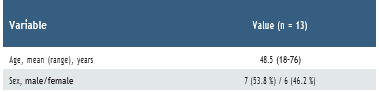
Table 2. Surgical approaches and outcomes in patients with giant hydatid cysts
Limitations
This study has several limitations that should be acknowledged. First, the retrospective and single-center design limits the generalizability of the findings, as patient selection and surgical decision-making may have been influenced by institutional practices and surgeon preference. Second, the relatively small sample size, particularly in the subgroup of patients undergoing laparoscopic surgery, restricts the statistical power to detect subtle differences in outcomes between surgical approaches. Third, the follow-up period was limited, preventing a comprehensive evaluation of long-term recurrence rates and late complications. Finally, potential selection bias cannot be excluded, as patients with more complex cyst characteristics were more likely to be directed toward open surgery. Future prospective, multicenter studies with larger cohorts and longer follow-up are warranted to validate these results.
Conclusion
In conclusion, giant hydatid cysts remain surgically challenging due to their size and risk of complications. Our data add to the growing body of evidence suggesting that, while open surgery continues to be the standard and most reliable approach for complex or multiple cysts, laparoscopic surgery can represent a safe and less invasive alternative in carefully selected patients with favorable cyst localization. The observed trend toward shorter hospitalization with laparoscopy underscores its potential clinical benefits; however, the possibility of postoperative complications, such as biliary fistula or pulmonary events, must always be considered. Future prospective, multicenter studies with larger patient populations and longer follow-up are essential to validate these findings and to establish more precise criteria for surgical decision-making in giant hydatid cysts.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Hogea MO, Ciomaga BF, Muntean MM, Muntean AA, Popa MI, Popa GL. Cystic echinococcosis in the early 2020s: A Review. Trop Med Infect Dis. 2024;9(2):36.
-
Khan MI, Ali R, Ji D, et al. Investigating the epidemiology and socioecological dynamics of hydatid-like cysts within a specific endemic district. Animals (Basel). 2025;15(11):1617.
-
Acosta-Jamett G, Hernández FA, Castro N, et al. Prevalence rate and risk factors of human cystic echinococcosis: A cross-sectional, community-based, abdominal ultrasound study in rural and urban north-central Chile. PLoS Negl Trop Dis. 2022;16(3):e0010280.
-
İskurt Y, Yabaci Tak A, Destek S, Akcakaya A, Bulbuloglu E, Deger KC. Komplike karaciğer kist hidatiğinde yönetim: Tek merkez deneyimimiz [Management of complicated hepatic hydatid cysts: Our single-center experience]. Ulus Travma Acil Cerrahi Derg. 2025;31(6):531-9.
-
Weber TF, Junghanss T, Stojković M. Pulmonary cystic echinococcosis. Curr Opin Infect Dis. 2023;36(5):318-25.
-
Mihetiu A, Bratu D, Neamtu B, Sabau D, Sandu A. Therapeutic options in hydatid hepatic cyst surgery: A retrospective analysis of three surgical approaches. Diagnostics (Basel). 2024;14(13):1399.
-
Abdennadher M, Hadj Dahmane M, Zribi H, et al. Management of giant hydatid cysts: a tertiary centre experience. Cardiothorac Surg. 2021;29:11.
-
Ghannouchi M, Rodayna H, Ben Khalifa M, Nacef K, Boudokhan M. Postoperative morbidity risk factors after conservative surgery of hydatic cyst of the liver: a retrospective study of 151 hydatic cysts of the liver. BMC Surg. 2022;22(1):120.
-
Zaharie F, Valean D, Zaharie R, et al. Surgical management of hydatid cyst disease of the liver: An improvement from our previous experience? World J Gastrointest Surg. 2023;15(5):847-58.
-
Ahmadinejad M, Hashemi M, Azizallahi N. Evaluation of prognostic factors associated with postoperative complications following pulmonary hydatid cyst surgery. Open Respir Med J. 2020;14:16-21.
-
Imran M, Abid Khan M, Janas I, et al. Efficacy and safety of surgical techniques in the management of pulmonary hydatid disease: a retrospective cohort study. Cureus. 2025;17(4):e82575.
-
Omar ASM, Osman TA, El Barbary MG. Laparoscopic versus open surgical management of liver hydatid cyst: a retrospective study. Egypt J Surg. 2022;41(1):65-75.
-
Berhuni MS, Kaya V, Yönder H, et al. Comparison of the effectiveness and complications of PAIR, open surgery, and laparoscopic surgery in the treatment of liver hydatid cysts. Medicina (Kaunas). 2025;61(8):1351.
-
Sotomayor C, Reyes N, Briceño E, et al. Radical laparoscopic pericystectomy of a giant hepatic hydatid cyst. Cureus. 2024;16(10):e71674.
-
Elmoghazy W, Alqahtani J, Kim SW, Sulieman I, Elaffandi A, Khalaf H. Comparative analysis of surgical management approaches for hydatid liver cysts: conventional vs. minimally invasive techniques. Langenbecks Arch Surg. 2023;408(1):320.
-
Vâlcea S, Dumitriu BC, Beuran M, Feier CVI. Biliary complications after surgery for hydatid disease: A five-year experience in a tertiary care center. Healthcare (Basel). 2025;13(9):1077.
-
Masood PF, Mufti GN, Wani SA, et al. Comparison of laparoscopic and open surgery in hepatic hydatid disease in children: Feasibility, efficacy and safety. J Minim Access Surg. 2022;18(3):360-5.
-
Wang Z, Zhu HH, Yang JY, et al. Laparoscopic versus conventional open treatment of hepatic cystic hydatidosis: a systematic review and meta-analysis of cohort studies. Wideochir Inne Tech Maloinwazyjne. 2022;17(3):406-17.
-
Slavu IM, Munteanu O, Gheorghita V, et al. Laparoscopic management of abdominal echinococcosis: A technical report on surgical techniques and outcomes. Cureus. 2024;16(3):e56130.
-
Bayrak M, Altıntas Y. Current approaches in the surgical treatment of liver hydatid disease: single center experience. BMC Surg. 2019;19(1):95.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content, including study design, data collection, analysis and interpretation, writing, and some of the main line, or all of the preparation and scientific review of the contents, and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Malatya Turgut Özal University (Date: 2025-09-16, No: E-30785963-020-331201)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Fatih Gönültaş, Osman Gökhan Gökdere. Surgical approach and clinical outcomes in giant hydatid cyst cases. Eu Clin Anal Med 2025;13(Suppl 1):S15-18
Publication History
- Received:
- October 16, 2025
- Accepted:
- October 24, 2025
- Published Online:
- October 24, 2025
- Printed:
- October 25, 2025
