Efficacy and safety of different doses of remifentanil for monitored anesthetic care during transurethral resection
Remifentanil treatment in transurethral resection
Authors
Abstract
Aim We aimed to investigate the efficacy and safety of transurethral resection (TUR) under monitored anesthetic care (MAC) and the effective dose of remifentanil.
Materials and Methods In this prospective, randomized, controlled trial, 50 patients were randomized to undergo TUR under monitored anesthetic care MAC. Vital signs were recorded at baseline and at 1, 5, 10, 15, 20, 30, 40, 50, and 60 minutes after induction. During induction, all patients received propofol at 1 mg/kg/h and remifentanil at 0.25 µg/kg/h. Following induction, Group 1 received a remifentanil infusion at 3 µg/kg/h, and Group 2 received 6 µg/kg/h. The depth of anesthesia was monitored using bispectral index (BIS) monitoring. Intraoperative and postoperative side effects, surgeon satisfaction, propofol consumption (PC), and recovery time were also recorded.
Results In our study, effective sedation and analgesia were achieved in both groups. However, intraoperative depth of anesthesia (p = 0.03), postoperative recovery time (p = 0.017), and surgeon satisfaction (p = 0.019) were better in Group 2. Hemodynamic and side effects were similar between the groups (p > 0.05). No adverse events were observed in any patient that would negatively affect the surgical procedure. SpO₂ values were transiently lower in Group 1 at 1, 5, and 15 minutes, but these differences were not statistically significant. BIS scores in group 2 were statistically lower than group 1 at all measurement times (p = 0.02). Group 2 demonstrated significantly shorter awakening and recovery times.
Discussion We think that TUR procedures using both remifentanil doses can be preferred under MAC. Both regimens were safe and effective; however, Group 2 demonstrated better hemodynamic stability, deeper sedation, higher surgeon satisfaction, and faster recovery.
Keywords
Introduction
Transurethral resection of the prostate (TURP) syndrome is characterized by headache, restlessness, confusion, cyanosis, dyspnea, arrhythmia, hypotension, or seizures, which occur when large amounts of irrigation fluid from the venous sinuses enter the systemic circulation. General anesthesia or neuraxial blocks (± obturator nerve block), especially spinal anesthesia, are preferred in the treatment of TURP syndrome and in transurethral procedures due to the potential for obturator jerk. In contrast, MAC is typically not preferred in transurethral resection (TUR) [1, 2, 3]. In the literature, it is seen that this method is generally preferred in high-risk patients where other methods cannot be applied [1, 4]. However, these problems have decreased thanks to advances in technology such as bipolar diathermy, radiofrequency, laser, microwave thermotherapy, and the use of bispectral index (BIS). These advances have facilitated the use of MAC in TUR procedures [5, 6]. The overall mortality rate from TURP syndrome appears to be decreasing steadily. For example, 2.5% in 1962, 1.3% in 1974, 0.23% in 1989, and 0.10% in 2003 [7]. Today, this rate is between 0% and 0.25% [8]. In their retrospective study on 53,182 patients who underwent TURP surgery, Ayoub et al. reported that 2.8% of the patients were performed under MAC anesthesia and that this method had similar complication rates with other anesthesia methods [1].
MAC aims to increase patient comfort and surgical satisfaction through effective sedation and analgesia, especially in short-term and minimally invasive surgical procedures. It offers advantages over general anesthesia, such as less physiological disruption and faster recovery. Recent reports indicate that MAC is the primary choice in 10-30% of all surgical procedures [9]. It is predicted that TUR will be increasingly preferred in MAC in the future, especially in suitable bladder tumors and small prostate resections. Therefore, more research is needed in this area. In our literature review, we did not find any prospective study comparing the effectiveness and safety of different doses of remifentanil in patients who underwent TUR under MAC.
The aim of this study is to evaluate the feasibility of MAC in patients undergoing TUR and to evaluate the effectiveness and safety of two different doses of remifentanil.
Materials and Methods
Participants
This study was conducted as a randomized, controlled, and single- blind study at Gaziantep University Faculty of Medicine, Department of Anesthesiology. Fifty patients between the ages of 18 and 75 in the American Society of Anesthesiologists (ASA) I-III risk group who would undergo elective prostate TUR Surgery (TUR-P) or Bladder TUR Surgery (TUR-B) were included in the study.
Patients meeting the following criteria were excluded from the study; ASA IV-V patients, those for whom deep sedation/general anesthesia is contraindicated or those with a history of adverse events during sedation/anesthesia, those who are allergic to remifentanil, propofol and its components (e.g. soybean oil, glycerol, triglycerides), lecithin, sodium oleate and sodium hydroxide), participants who have taken part in any pharmacological clinical study in the last 3 months, breastfeeding or pregnant women, patients with a body mass index >35 kg/m2, patients with a prostate size >50 cc, and patients with other conditions that we consider unsuitable for this study (e.g. opioid addicts and chronic analgesic users).
Verbal and written informed consent was obtained from all patients before surgery. The patients were randomized by the sealed envelope method and divided into two groups, Group 1 and Group 2, with equal numbers of patients.
Application and sedation protocol
All patients fasted for at least 8 hours before surgery and were premedicated with intravenous 1-2 mg midazolam before the procedure. Age, gender, weight, type of surgery, and ASA scores were recorded before the procedure. Heart rate (HR), systolic (SAP), diastolic (DAP), and noninvasive mean blood pressure (MAP), peripheral O2 saturation (SpO2), and respiratory rate (RR) were monitored. 8 mL/kg/h i.v. Isotonic NaCl infusion was started. BIS monitoring (Aspect Medical Systems, A-2000 BIS Monitor, Netherlands) was used to determine the depth of anesthesia.
HR, MAP, SpO2, RR, and BIS values were recorded before induction, after induction, and at 1, 5, 10, 15, 20, 30, 40, 50, and 60 minutes of remifentanil infusion. After the control values were taken, the patients were given 4 lt/min 100% O2 via nasal cannula. Infusions of 10 mg/kg/h for propofol (B. Braun Melsungen, Propofol Lipuro 1%, Germany) and 20 µg/kg/h for remifentanil (GlaxoSmithKline, Ultiva 5 mg vial, Italy) were prepared and administered.
All patients were induced with 1 mg/kg/h propofol and 0.25 µg/kg/h remifentanil. Afterwards, 3 mg/kg/h propofol infusion was started. Following induction of anesthesia, patients were randomly divided into two groups before surgery; Group 1 (n = 25) was given 3 µg/kg/h remifentanil, and Group 2 (n = 25) was given 6 µg/kg/h remifentanil.
Patients with a BIS score of 75-85 after induction were placed in the lithotomy position. At least 10 minutes before induction, local anesthesia was applied to the urethra with 20 ml of sterile lubricating gel (Aqua Touch, Lidocaine 2% Gel, Ankara, Turkey).
A propofol bolus dose of 0.4 mg/kg/h was administered to both groups every 3 minutes until the target BIS score (60-75) was reached, and the infusion rate was increased by 0.5 mg/kg/h. At values below the target BIS score, the propofol infusion rate was reduced by 0.5 mg/ kg/h. Remifentanil infusion was not interrupted during the operation. Additional doses of propofol were similarly administered to patients who showed movement during the procedure.
Our primary aim in the study was to investigate whether the procedures would be performed successfully and to measure the surgeon’s satisfaction level. Success is defined as completing the procedure without the need for general anesthesia and without the need for more than 5 doses of additional anesthesia within 15 minutes.
Secondary outcomes were to compare the effectiveness and safety of anesthesia. In terms of effectiveness, vital signs, sedation levels, time to reach target sedation, amount of additional dose administered throughout the procedure, and cumulative dose were evaluated in both groups. Safety, recovery times, movement during the procedure, drug-related adverse events (respiratory, such as desaturation, hypoxia, bronchospasm, cough, intubation, or cardiovascular, such as bradycardia, arrhythmia, hypertension, hypotension, inotropic need) were evaluated.
Before induction, preparations were made against all possible side effects. A decrease in SpO2 below 95% during the operation was defined as “desaturation”, and a decrease below 90% was defined as “hypoxia”. When desaturation was observed in the patient, first tactile and verbal warnings were given, and then, depending on the situation, the jaw thrust maneuver was applied and the airway was entered. If there was no improvement within 1 minute despite this intervention, mask ventilation with 100% O2 was planned. In case of hypoxia, mask ventilation was applied. Mask ventilation times were recorded. If there was no improvement despite these attempts, laryngeal mask placement or intubation was planned.
No intervention was planned for patients with a heart rate ≤ 50 bpm, as long as it did not adversely affect blood pressure. When MAP was <60 mmHg or 25% lower than control MAP, 5 mg ephedrine was administered intravenously and repeated every 3-5 minutes if necessary. It was planned to give 0.01 mg/kg atropine to patients with resistant bradycardia (HR <50 beats/min). In resistant hypotension, it was planned to increase the crystalloid fluid infusion rate to 10 ml.kg-1 and then start dopamine infusion. After the resectoscope was removed from the urethra, propofol and remifentanil infusions were terminated, and total propofol and remifentanil doses, anesthesia, and operation times were recorded.
When the patients responded to verbal stimuli after the procedure, they were transferred to the postoperative recovery room, and when the Aldrete score was ≥ 9, that is, there was a recovery period, they were transferred to the patient rooms (10). Eye-opening time with verbal stimulation was defined as the waking time. After the operation was completed, the operating surgeon (who was blind to the groups) was asked to score anesthesia satisfaction from 1 to 4 (very good: 4, good: 3, moderate: 2, bad: 1) (Figure 1).
Statistical analysis The estimated sample size was calculated based on the difference between satisfaction scores in a previous study (3.41 ± 0.80 vs. 2.36 ± 1.26) [10]. We assumed that the expected difference in satisfaction scores was greater than 1, and in accordance with this assumption, a minimum of 20 patients per group was required. To achieve this, 25 patients were recruited for each group, and ultimately, 25 patients per group completed the study. The Kolmogorov-Smirnov test was used to check the suitability of continuous variables for normal distribution. In univariate analysis, the Student T test was used to compare normally distributed variables in two independent groups, and the Mann- Whitney U test was used for non-normally distributed variables. The relationship between categorical variables was tested with chi-square analysis. Repeated measures ANOVA was used to compare repeated measures, and two-way ANOVA was used to evaluate multiple factors together. Frequency, percentage, and mean ± SD values were given as input statistics. SPSS for Windows v.22 was used in statistical analysis, and a p-value of <0.05 was considered statistically significant.
Ethical approval
Ethical approval was received from the Gaziantep University local ethics committee (Date: 2013-09-17, No: 17.09.2013/323).
Results
Comparison of demographic values is shown in Table 1. There was no statistically significant difference between the groups in terms of demographic data (p > 0.05). Comorbidities in both groups were hypertension, diabetes, chronic obstructive pulmonary disease, and kidney disease. The average prostate size in TURP surgery was determined to be 40 grams (range 30-50 grams) (Table 1).
Primary Results
There was no statistical significance between the groups in terms of hemodynamic values (p > 0.05) (Figure 2). The procedures in both groups were completed successfully in all patients, and no patient required intubation or advanced airway equipment. However, oxygen saturations were similar (p > 0.05) (Figure 3). Sedation levels (BIS Score) in group 2 were statistically lower than group 1 at all measurement times (p = 0.02) (Figure 3). Target sedation scores (BIS 60-75) were reached in both groups.
Vital signs (HR, MAP, RR, SPO2) were similar in both groups, and there was no statistical difference except for some measurement times (p > 0.05). However, patients in Group 2 were clinically more stable (Table 2).
Secondary Results
Intraoperative adverse events were comparable between the two groups. The incidence of desaturation (SpO₂ < 95%) was 14 cases in Group 1 and 12 cases in Group 2 (p = 0.39), while hypoxemia (SpO₂ < 90%) occurred in 10 and 6 patients, respectively (p = 0.77). Bradycardia (HR < 60 beats/min) was observed in 2 patients in Group 1 and 6 patients in Group 2 (p = 0.15). No hypotensive episodes (MAP < 60 mmHg) were recorded in either group. Hypertension (MAP 100–120/> 120 mmHg) occurred in 7 and 1 patients in Group 1, and 4 and 1 patients in Group 2 (p = 0.36). The proportion of patients requiring respiratory support with a mask was 12 in Group 1 and 18 in Group 2 (p = 0.86). The mean duration of respiratory support was 11.67 ± 9.37 minutes in Group 1 and 11.39 ± 8.36 minutes in Group 2, with no statistically significant difference between the groups (p = 0.88).
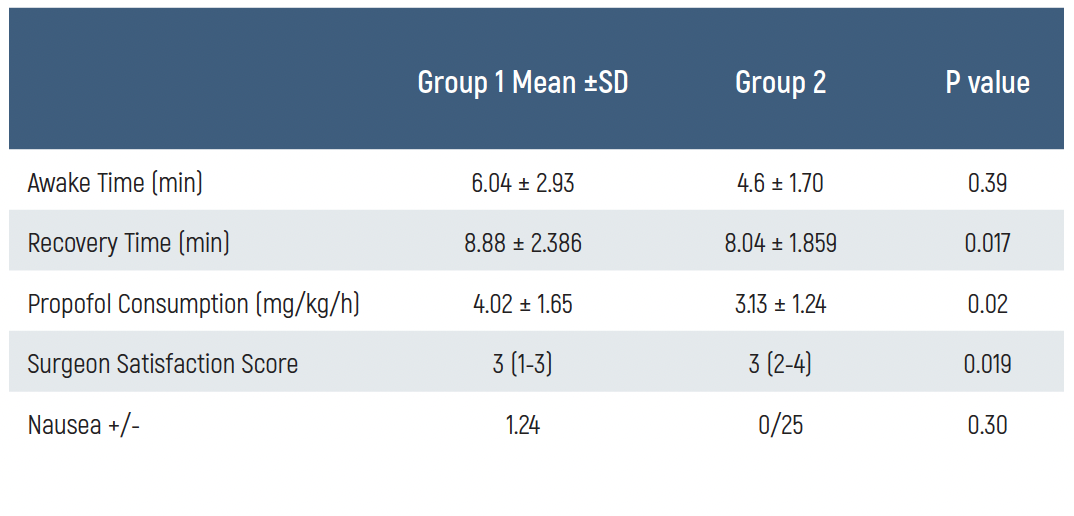
Comparison of postoperative measurement values is shown in Table 3. Awakening time was similar between groups (6.04 ± 2.93 min vs. 4.6 ± 1.70 min, p = 0.39). In contrast, recovery time differed significantly, being longer in Group 1 (8.88 ± 2.39 min) compared to Group 2 (8.04 ± 1.86 min, p = 0.017). Propofol consumption was higher in Group 1 (4.02 ± 1.65 mg/kg/h) than in Group 2 (3.13 ± 1.24 mg/kg/h), and the difference was statistically significant (p = 0.02). Surgeon satisfaction scores were slightly higher in Group 2 (median 3, range 2–4) compared to Group 1 (median 3, range 1–3), with a significant difference (p = 0.019). The incidence of postoperative nausea was low and similar between the groups (1/24 in Group 1 vs. 0/25 in Group 2; p = 0.30) (Table 3).
Discussion
To our knowledge, this is the first prospective, randomized controlled trial to directly compare different doses of remifentanil for MAC during TUR procedures. In this study, we aimed to reveal the applicability of MAC in TUR, and the optimum dose of remifentanil was investigated.
Our study is the first randomized controlled trial of TURP/B with MAC anesthesia. TUR under local anesthesia and sedation was first reported by Moffat et al. [11]. In this study, it was reported that the method was well tolerated by the patients and no major complications were observed. Acceptable success rates were reported in many similar studies conducted in subsequent years [12, 13, 14, 15]. Miroglu et al. reported an 82% success rate in the TUR procedure with this method [12]. Sinha et al. reported that 87% of patients were satisfied with this procedure [16]. These studies underlined that it is a good alternative to general and regional anesthesia, especially in high-risk patients [3, 5, 15, 16]. Currently, the procedure is successfully applied to selected patients in some clinics, as reported in previous studies [1, 4, 8, 9]. A recent retrospective study on 52,182 patients reported that TUR-P under MAC had similar complication rates as general and spinal anesthesia in patients with advanced age, high ASA, diabetes, and COPD [1].
Our study is different from previous studies in that only intraurethral 2% lidocaine gel was used as a local anesthetic, and it was performed with deeper sedation under BIS guidance. Although it has been reported that lidocaine 2% gel alone is sufficient for endoscopic urological procedures, it may not provide sufficient analgesia for TUR alone [17]. Therefore, it should be combined with effective sedatives and analgesics. It is important that the sedation level is at the depth required for the surgery and that those side effects, especially respiratory and hemodynamic effects, are avoided. We tried to achieve this balance with BIS monitoring.
Many different anesthetic/analgesic agents can be used in MAC [18, 19]. The anesthetics to be preferred and their doses vary depending on the patient’s health condition and/or the surgical procedure to be performed. The fact that remifentanil is a powerful analgesic and has a short dose-independent half-life has made this drug the preferred analgesic agent in MAC [20, 21]. Propofol, like remifentanil, is a short- acting anesthetic agent, and these two agents complement each other pharmacodynamically. Vuyk et al. reported that remifentanil added to propofol is superior to other opioids in terms of recovery time [22].
In a study investigating the effect of remifentanil added to propofol on the depth of sedation with BIS monitoring, it was reported that faster and deeper sedation levels were achieved with remifentanil added to propofol and that remifentanil doses of 3 microgr.kg.h-1 were compared to 6 microgr.kg.h-1. They said it caused fewer side effects. In this study, fixed-dose propofol infusion was applied [23]. However, determining the optimum drug combination and dosage for each surgical procedure is a matter of research. The use of propofol and/ or remifentanil in endoscopic urological procedures has been reported [24]. The number of studies on transurethral resection is very limited. Verdejo et al. reported that propofol-remifentanil infusion was used for sedation in addition to local anesthesia in ASA III-IV patients with benign prostatic hypertrophy who underwent TUR. As a result, they reported that there were no complications arising from anesthesia [25]. However, in the aforementioned study, all patients were administered a fixed dose of remifentanil, and no comparison of different doses was made.
When the hemodynamic status was evaluated in our study, it was seen that anesthesia was more stable in Group 2. It has been reported that high doses and rapid administration of propofol and remifentanil during induction cause bradycardia and hypotension, but low doses and/or slow (e.g., infusion) administration of these drugs have less effect on hemodynamics [19, 21, 22]. For induction, we started with lower doses of propofol and remifentanil (1 mg/kg propofol, 0.25 µg/ kg remifentanil). While remifentanil was continued as an infusion at different doses, additional doses of propofol were administered according to the BIS index. In this way, none of our patients (including our ASA 3 and 4 patients) experienced hypotension or bradycardia requiring intervention. Although the decrease was more pronounced in Group 2, it remained within clinically acceptable limits.
Both propofol and remifentanil have respiratory suppressant properties. In our study, transient desaturation and hypoxia occurred in both groups but were managed with simple airway maneuvers, and no patient required intubation. Importantly, BIS monitoring allowed titration to adequate depth while minimizing respiratory compromise. As it is known, BIS is a device that measures the depth of anesthesia with the help of brain waves and thus facilitates the MAC technique in critical situations [23]. Studies have reported that BIS monitoring reduces anesthesia consumption, complications, and recovery time by optimizing the depth of anesthesia. Despite this, respiratory depression was observed in both groups. However, this period was short-lived, and no patient required long-term mask ventilation or intubation. There was no difference between the groups in terms of the number of breaths and duration of support.
In our study, eye opening and recovery were faster in Group 2 (p > 0.05). The most important reason for this is that the remifentanil dose in this group provided a more effective analgesia, so hypnotics were used less. The positive effects of effective analgesia on postoperative recovery have been reported in many studies. It was reported that patients who used propofol + remifentanil had earlier recovery than those who used propofol alone [23]. Other studies had similar results [5, 20, 22]. Our recovery time findings are consistent with prior reports. Verdejo et al. demonstrated safe and complication-free use of propofol–remifentanil sedation in high-risk TUR patients, and Vuyk et al. showed that remifentanil added to propofol shortened recovery compared to other opioid combinations. Similarly, we observed that higher-dose remifentanil (Group 2) was associated with faster recovery and reduced propofol consumption.
Figures

Figure 1
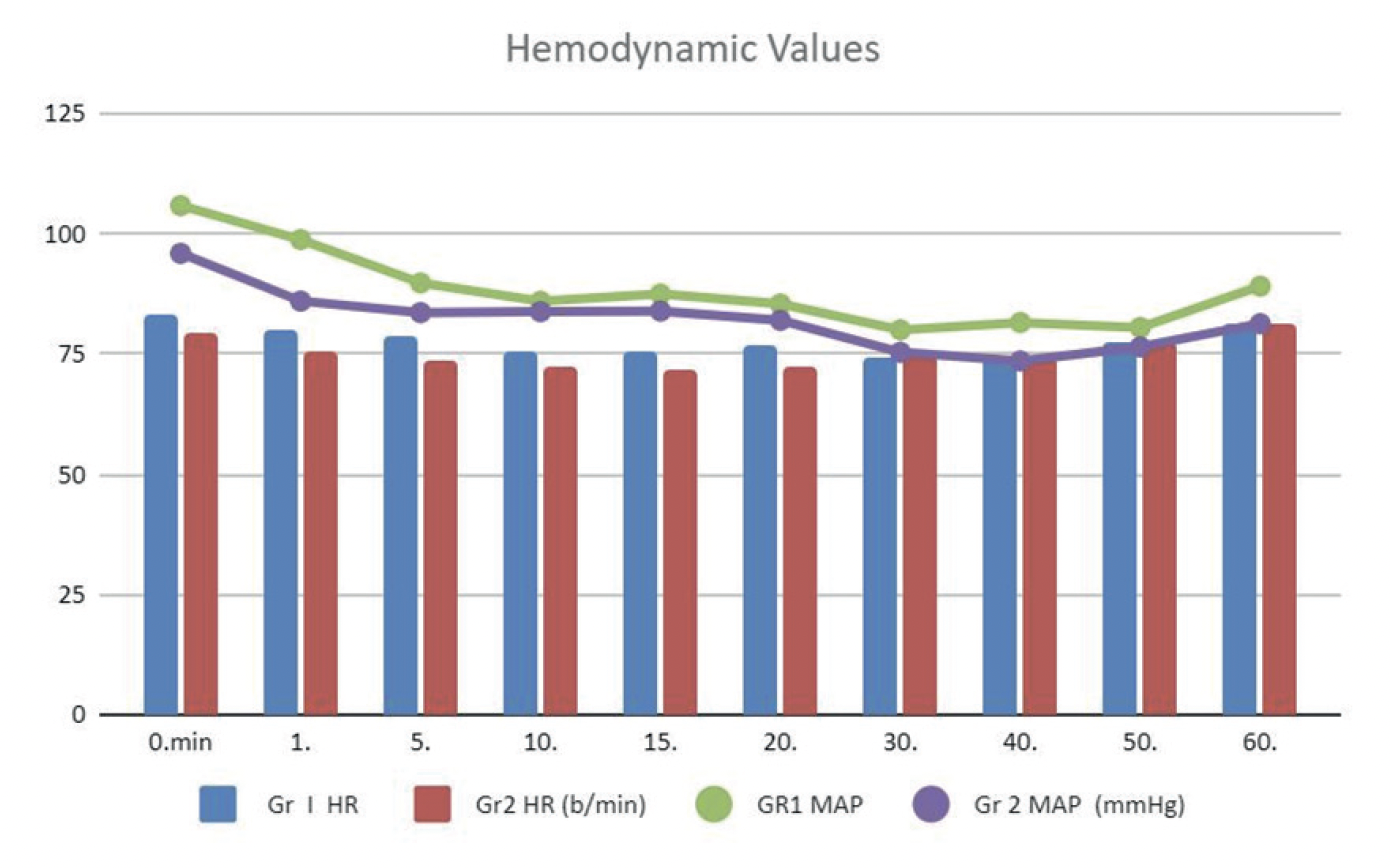
Figure 2

Figure 3
Tables
Table 1
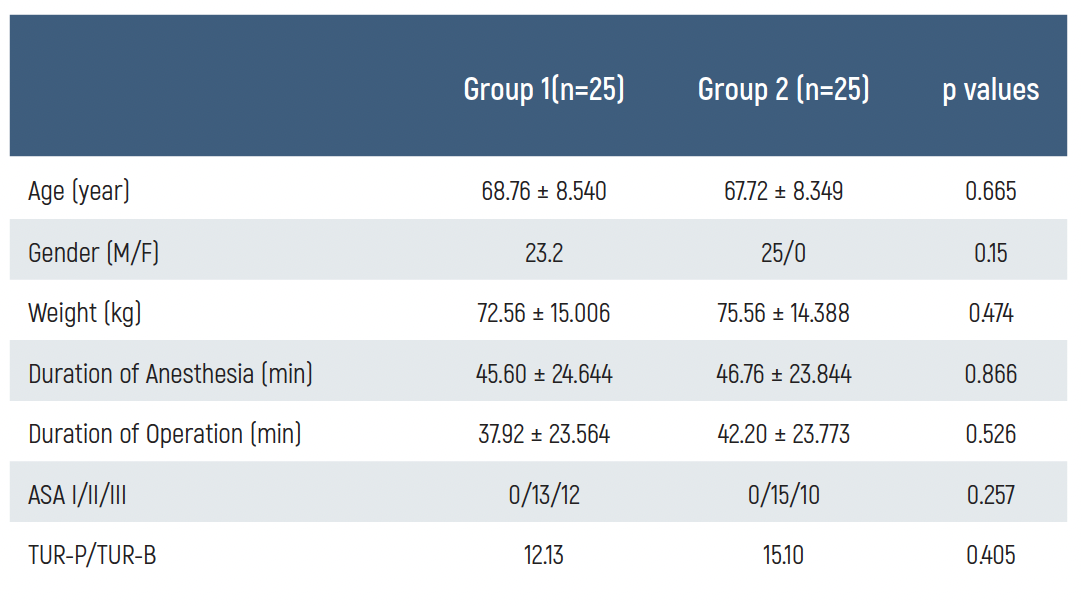
Table 2
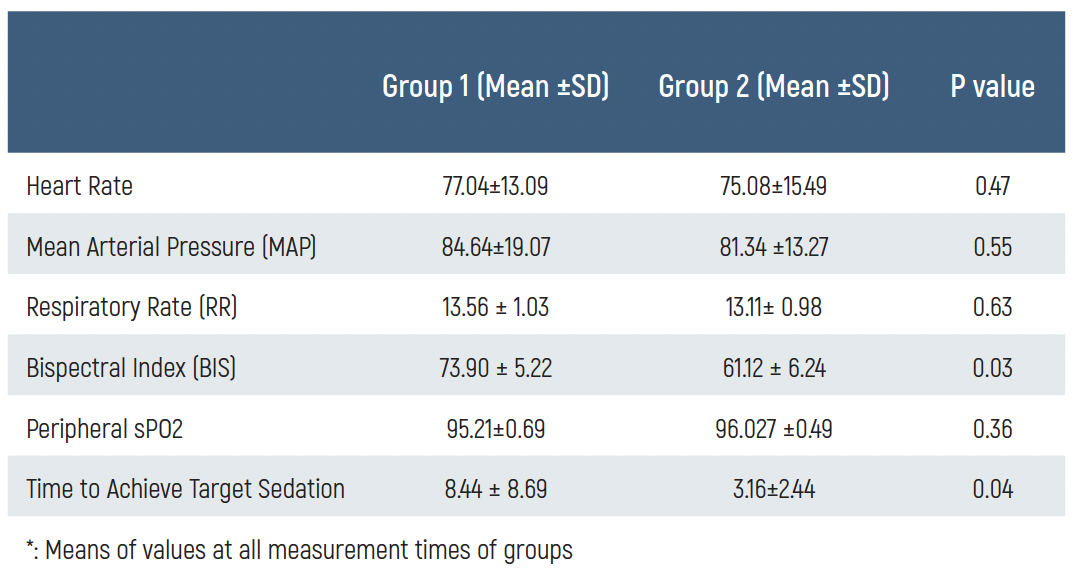
Table 3
Limitations
This study has some limitations. Although the study was adequately powered for the primary endpoint, the relatively small sample size may limit generalizability. The trial was conducted in a single center, potentially introducing center-specific biases. Additionally, the follow- up period was limited to the intraoperative and early postoperative phases, preventing assessment of long-term outcomes or late complications. Finally, factors such as inter-individual variability in anesthetic response and surgeon experience, which may influence the results, were not fully controlled.
Conclusion
In conclusion, this study showed that both drug combinations provided adequate MAC anesthesia for TUR procedures, but the quality of intraoperative sedation and analgesia and the postoperative recovery rate were higher in Group 2. Both doses appear to be feasible options for MAC in urological endoscopic interventions; however, the higher dose provided superior outcomes in our trial.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Ayoub CH, Chalhoub V, El-Achkar A, et al. Sedation as an alternative anesthetic technique for frail patients in transurethral resection of the prostate. Ther Adv Urol. 2023;15(1):1-12.
-
van Kollenburg RAA, van Riel L, de Bruin DM, de Rijke TM, Oddens JR. Novel minimally invasive treatments for lower urinary tract symptoms: a systematic review and network meta-analysis. Int Braz J Urol. 2023;49(4):411-27.
-
Wong K, Kinsella N, Seth J, et al. Comparing urolift and standard transurethral resection of prostate ahead of radiotherapy in men with urinary symptoms secondary to prostate enlargement in southwest london and north cumbria (CO-STAR): a study protocol for a randomised feasibility study. BMJ Open. 2023;13(10):1-9.
-
Guerra A, Chao C, Wallace GA, Rodriguez HE, Eskandari MK. Changes in anesthesia can reduce periprocedural urinary retention after EVAR. Ann Vasc Surg. 2022;79(2):91-9.
-
Nagata O, Matsuki Y, Matsuda S, et al. Anesthesia management via an automated control system for propofol, remifentanil, and rocuronium compared to management by anesthesiologists: an investigator-ınitiated study. J Clin Med. 2023;12(20):6611-19.
-
Roberts WW. New technologies in benign prostatic hyperplasia management. Curr Opin Urol. 2016;26(3):254-8.
-
Evrard PL, Mongiat-Artus P, Desgrandchamps F. [Morbi-mortality of transurethral resection of the prostate in patients aged 75 and over]. Prog Urol. 2017;27(5):312-8.
-
Agrawal MS, Mishra DK. Transurethral resection of prostate. J Endourol. 2022;36(2):29-34.
-
Howell SJ, Absalom AR. Consensus guidelines, Delphi methods, and evidence around anaesthetic technique for endoscopic retrograde cholangiopancreatography. Br J Anaesth. 2023;131(4):634-6.
-
Erdurmus M, Aydin B, Usta B, Yagci R, Gozdemir M, Totan Y. Patient comfort and surgeon satisfaction during cataract surgery using topical anesthesia with or without dexmedetomidine sedation. Eur J Ophthalmol. 2008;18(3):361-7.
-
Moffat NA. Transurethral prostatic resections under local anesthesia. J Urol. 1977;118(4):607-8.
-
Miroglu C, Saporta L. Transurethral ureteroscopy: is local anesthesia with intravenous sedation sufficiently effective and safe? Eur Urol. 1997;31(1):36-9.
-
Pula R, Gooty S, Thakur N, Sharathchandra B. Dural sac cross-sectional area measured using ultrasound to modify the dosage of local anaesthetic in spinal anaesthesia for transurethral resection of prostate surgery: a prospective, double blind, randomised controlled study. Indian J Anaesth. 2022;66(10):719-23.
-
Krishan A, Bruce A, Khashaba S, Abouelela M, Ehsanullah SA. Safety and efficacy of transurethral resection of bladder tumor comparing spinal anesthesia with spinal anesthesia with an obturator nerve block: a systematic review and meta-analysis. J Endourol. 2021;35(3):249-58.
-
Wang H, Deng W, Zhu X, Fei C. Perioperative analgesia with ultrasound-guided quadratus lumborum block for transurethral resection of prostate. Medicine (Baltimore). 2021;100(51):e28384.
-
Sinha B, Haikel G, Lange PH, Moon TD, Narayan P. Transurethral resection of the prostate with local anesthesia in 100 patients. J Urol. 1986;135(4):719-21.
-
Aaronson DS, Walsh TJ, Smith JF, Davies BJ, Hsieh MH, Konety BR. Meta-analysis: does lidocaine gel before flexible cystoscopy provide pain relief? BJU Int. 2009;104(4):506-9.
-
Okano H, Kataoka Y, Sakuraya M, et al. Efficacy of remifentanil in patients undergoing cardiac surgery: a systematic review and network meta-analysis. Cureus. 2023;15(12):e51278.
-
Koruk S, Koruk I, Arslan AM, Bilgi M, Gul R, Bozgeyik S. Dexmedetomidine or midazolam in combination with propofol for sedation in endoscopic retrograde cholangiopancreatography: a randomized double blind prospective study. Wideochir Inne Tech Maloinwazyjne. 2020;15(3):526-32.
-
Stasiowski MJ, Zmarzly N, Grabarek BO, Gasiorek J. Postoperative nausea and vomiting following endoscopic sinus surgery under the guidance of adequacy of anesthesia or pupillometry with ıntravenous propofol/remifentanil. Pharmaceuticals (Basel). 2023;17(1):1-9.
-
Hernando Vela B, Jaren Cubillo P, Bueno Fernandez C, Gallego Ligorit L, Ferrer Garcia MC, Diarte JA. Sedation with propofol/remifentanil versus dexmedetomidine / remifentanil for patients undergoing transcatheter aortic valve implant: a retrospective study between 2012 and 2019. Rev Esp Anestesiol Reanim (Engl Ed). 2023;71(2):68-75.
-
Vuyk J, Mertens MJ, Olofsen E, Burm AG, Bovill JG. Propofol anesthesia and rational opioid selection: determination of optimal EC50-EC95 propofol-opioid concentrations that assure adequate anesthesia and a rapid return of consciousness. Anesthesiology. 1997;87(6):1549- 62.
-
De Vico P, Biasucci DG, Aversano L, et al. Feasibility and safety of deep sedation with propofol and remifentanil in spontaneous breathing during endoscopic retrograde cholangiopancreatography: an observational prospective study. BMC Anesthesiol. 2023;23(1):260-68.
-
Tschirdewahn S, Rubben H, Schenck M. Urological surgery with analogosedation and local anesthesia. What makes sense? Urologe A. 2013;52(9):1302-11.
-
Navalon Verdejo P, Sanchez Ballester F, Ordono Dominguez F, Pallas Costa Y, Juan Escudero J, Canovas Ivorra JA. Endoscopic treatment of the benign prostatic hyperplasia with local anesthesia and sedation in patients with high surgical or anaesthesical risk. Actas Urol Esp. 2006;30(1):46-51.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Gaziantep University (Date: 2013-09-17, No: 17.09.2013/323)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Aziz Yarbil, Rauf Gul, Vahap Saricicek, Levent Sahin, Metin Kilinc, Ergun Mendes, Huseyin Gocergil, Muharrem Baturu. Efficacy and safety of different doses of remifentanil for monitored anesthetic care during transurethral resection. Eu Clin Anal Med 2025;13(3):70-74
Publication History
- Received:
- August 13, 2025
- Accepted:
- August 31, 2025
- Published Online:
- August 31, 2025
- Printed:
- September 1, 2025
