Intramedullary nailing outcomes in open fractures due to firearm injuries
Nailing in open fracture
Authors
Abstract
Aim This study aims to evaluate the outcomes of intramedullary nailing (IMN) in open fractures due to firearm injuries and analyze differences in healing time, infection rates, and hospital stay durations among femur, tibia, and humerus fractures.
Material and Methods A retrospective study was conducted on 89 patients treated with IMN for open fractures caused by firearm injuries. Patients were classified by the affected bone, and variables including healing time, nonunion, infection rates, and hospital stay were assessed.
Results The mean healing time was 19 weeks for femur fractures, 22 weeks for tibia fractures, and 10.1 weeks for humerus fractures. Tibia fractures had the highest infection rate (17.6%), followed by the humerus (14.3%) and femur fractures (10.4%). Nonunion was observed in 3 femur and 3 tibia cases, while humerus fractures had no nonunion. Patients with tibia fractures also had the longest mean hospital stay.
Discussion Intramedullary nailing (IMN) is an effective treatment for gunshot-induced fractures, particularly for femoral and humeral fractures. Our study showed similar union times to previous studies, though high-velocity injuries were linked to higher delayed union and infection rates. Tibial fractures, more prone to infection, showed lower delayed union rates, possibly due to unreamed IMN. However, infection remains a significant concern, especially in war-related injuries. In conclusion, while IMN offers favorable outcomes for gunshot fractures, high infection rates in high-velocity injuries underscore the need for further research to refine treatment strategies, especially for severe fractures.
Keywords
Introduction
Fractures related to firearm injuries represent a distinct type of open fracture. These fractures pose significant challenges for orthopedic surgeons. Three-quarters of all injuries occur in the extremities during modern warfare. More than one-third of these injuries are associated with bone fractures [1].
Around 40% of gunshot injuries affect the lower extremities, with the femur being the most affected bone [2, 3]. As with all open fractures, the goals of treatment for femoral open fractures are to prevent infection, promote fracture healing, and restore the previous functions of the injured extremity [3, 4, 5]. Acceptable infection rates and appropriate healing times have been reported for low-velocity gunshot injuries treated with simple debridement and early closed intramedullary nailing [6, 7]. However, a definitive treatment protocol for high-velocity gunshot injuries has not yet been established, and there is insufficient literature on this topic [8].
This study aims to determine the effect of early intramedullary nailing on fracture healing and the development of complications in long bone fractures such as femur, tibia, and humerus following gunshot injuries, comparing these outcomes with existing literature data.
Materials and Methods
The study was initiated with the approval of the Mustafa Kemal University Ethics Committee. A total of 89 patients with Gustilo Anderson type 3a open femoral, tibial, and humeral shaft fractures secondary to high- velocity gunshot injuries during the Syrian civil war and with a minimum follow-up of 6 months were included in the study. Subtrochanteric, intertrochanteric, and supracondylar fractures and Gustilo Anderson type 3b and type 3c fractures were not included in the study.
Patients received a combination of first-generation cephalosporin and aminoglycoside intravenously for 72 hours for prophylaxis. Upon arrival at the emergency department, open wounds were irrigated, the surrounding area was cleaned with betadine, covered with sterile dressings, and splinted, and antibiotic prophylaxis was initiated. Radiological evaluations were performed, and the diagnosis was confirmed with full AP and lateral radiographs including one joint above and one joint below the fracture site. Informed written consent for intramedullary nailing was obtained from all patients. Patients were operated on under spinal anesthesia, and antegrade locked intramedullary nails were used in the surgeries. Debridement was performed along the bullet tract, and routine cultures were taken.
Patients were provided with parenteral analgesic and anti-inflammatory treatment in the postoperative period, and narcotic analgesics were administered if necessary. Starting from the first postoperative day, knee bending, ankle, shoulder, and elbow exercises were initiated. Patients with stable general conditions were mobilized on the first postoperative day without full weight bearing and were instructed to walk with crutches. Dressings were performed daily, and patients were scheduled for suture removal on the 15th day and follow-up visits on the 3rd and 6th weeks for evaluation of healing status, joint movements, and weight-bearing.
Statistical Analysis
SPSS 25.0 package program was used for statistical analysis. Categorical measurements were summarized as numbers and percentages, and continuous measurements were summarized as median and minimum-maximum. The Chi-square test or Fisher’s exact test was used for comparing categorical variables. Mann-Whitney U test was used for comparing continuous measurements between groups, and the Kruskal-Wallis test was used for comparing more than two variables. A statistical significance level of 0.05 was considered for all tests.
Ethical Approval
This study was approved by the Ethics Committee of Mustafa Kemal University for non-interventional clinical research (Date: 2020-11-12, No:19).
Results
A total of 89 patients who presented to the Hatay Mustafa Kemal University Faculty of Medicine Research Hospital Orthopedics and Traumatology Clinic between 2008 and 2019 due to gunshot injuries and completed their treatment were retrospectively evaluated. All 89 patients injured in the Syrian civil war were male. Of these patients, 48 had femoral, 34 had tibial shaft, and 7 had humeral shaft fractures, all of which were treated with intramedullary nails.
The mean age of the 48 patients with femoral fractures was 31.5 years. The average duration of surgery for these patients was 3.5 hours. Forty-four patients had high-velocity, while 4 had low-velocity gunshot injuries. Thirty-four patients were smokers. The average time to union was 19.2 weeks (range 15-44 weeks). Ten patients started full weight- bearing walking after the 3rd postoperative week, 30 patients after the 6th postoperative week, and the remaining patients started later. Five patients developed postoperative infections (10.41%). Two of these (4.1%) were superficial infections characterized by discharge and erythema of the wound edges within the first 2 weeks postoperatively(Table 1,2,3). These infections resolved after debridement. Deep infection developed in the remaining 3 patients (6.25%). In one case, the infection regressed after debridement, but in 2 cases (4.1%), the discharge became chronic, and osteomyelitis developed.
Patient with femoral fractures- Nonunion was observed in a total of 3 patients (6.25%). One of them had osteomyelitis. Union was achieved after pseudoarthrosis surgery in these patients. Delayed union occurred in six patients (12.5%). Union was achieved after dynamization in four patients. Delayed union was associated with deep infection in the other two patients, and union was achieved after infection treatment. Limb shortening was observed in three patients (2 patients with 2 cm, 1 patient with 1 cm) (Table 1).
The mean age of the 34 patients with tibial fractures was 34.8 years, with an average surgery duration of 4.2 hours. Two patients had low-velocity, while 32 had high-velocity gunshot injuries. Twenty-two patients were smokers. The mean time to union for the 32 patients who achieved union was 22 weeks (range 15-40 weeks). Delayed union was observed in five patients (14.7%) (28-40 weeks), and union was achieved after distal dynamization in 2 patients. In the other 3 patients, the delayed union was associated with deep infection. Union was achieved after infection resolution (Table 2).
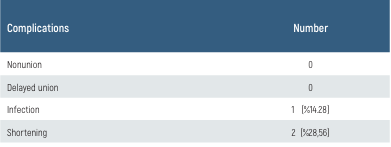
The average surgery duration for the seven humeral fractures was 2.14 hours (range 1.5-3 hours). The mean time to union was 10.1 weeks (range 8-12 weeks). One of the seven humeral fractures (14.2%) resulted from low-velocity, while six were due to high-velocity gunshot injuries. All patients had isolated humeral fractures, and all were smokers.
One patient (14.28%) developed an early superficial infection in the postoperative period, leading to debridement. After debridement, antibiotic therapy, and dressing changes, the infection resolved. No patient developed a deep infection, and there were no cases of nonunion (Table 3).
In a total of 29 smoking patients, it was observed that smoking had an effect on nonunion, delayed union, and infection development. It was observed that the rate of infection was significantly higher in the smoking group compared to the non-smoking group (p=0.006). Similarly, the rate of delayed union was found to be significantly higher in smokers (p=0.012). Although the rate of nonunion was also higher in the smoking group compared to the non-smoking group, this result was not statistically significant (p=0.147)
The effect of surgery duration on the development of complications was evaluated. As the duration of surgery increased in patients, the rates of complications also significantly increased (p=0.005). Prolonged surgery duration was observed to increase the infection rate significantly (p=0.004). Similarly, the rate of delayed union significantly increased with the prolonged duration of surgery (p=0.003). However, no statistically significant relationship was found between the duration of surgery and nonunion (p=0.716).
Discussion
In gunshot injuries, as with all fractures, the type of fracture, the condition of soft tissue, the localization of the fracture, the presence of accompanying traumas, and the experience of the treating physician may lead to the preference for one of the methods such as external fixation, plate and screw osteosynthesis, and intramedullary nailing [11]. Factors such as the comminution zone can be crucial in deciding on the fixation method, as noted by Hilton et al. External fixation is recommended for gunshot fractures of the tibia when the radiological fragmentation area exceeds 120 mm [12]. However, we did not perform radiographic measurements of the comminution zone in our series. The use of intramedullary nailing in complex femoral fractures occurring after gunshot injuries has been considered since the 1940s due to reasons such as nonunion and malunion [13, 14]. Hollman and colleagues stated that they applied intramedullary nailing in a single stage to 19 femoral fractures resulting from low-velocity gunshot injuries and calculated the average union time as 4.5 months (20 weeks). Nonunion occurred in one patient (5.2%), and delayed union occurred in one patient (5.2%) [15]. Our study yielded similar results in terms of union time and nonunion rates. We observed delayed union in 6 patients (12.5%). We attribute these high rates of delayed union to the majority of cases being caused by high-velocity, long-barreled firearms.
In a study conducted by Mian Amjad Ali and colleagues involving 68 patients with femoral fractures resulting from high-velocity gunshot injuries treated with locked intramedullary nails, the average union time was reported as 24 weeks, with nonunion observed in 4 cases (5.88%) [16]. We applied intramedullary nailing to 48 femoral shaft fractures, the majority of which occurred as a result of high-velocity gunshot injuries, and calculated the average union time as 19.2 weeks. Nonunion was observed in 3 patients (6.25%). We attribute this relatively shorter union time to the young patient profile, early weight bearing, and our experience in war surgery.
On the other hand, Hollmann et al. reported one case (5.2%) of infection in a femoral fracture treated with intramedullary nailing [17]. Bergman and colleagues, in a series of 65 femoral fractures resulting from gunshot injuries and treated with intramedullary nailing, observed serous drainage that regressed with 2-3 weeks of antibiotic therapy in 2 cases (3%) [11]. Tornetta did not observe deep infection in femoral shaft fractures treated with intramedullary nailing after gunshot injuries, but one patient developed cellulitis [18]. However, all the aforementioned authors mainly examined femoral fractures resulting from low-velocity gunshot injuries in their studies. Since the majority (91.6%) of femoral fractures in our study occurred as a result of high-velocity gunshot injuries, we believe that our infection rates were higher.
In the series by Mian Amjad Ali et al., 7 out of 68 patients (10.29%) with femoral fractures resulting from high-velocity gunshot injuries developed infections, with 3 (4.4%) being superficial and 4 (5.88%) being deep infections [16]. Similarly, in our study, we detected superficial infections in 2 patients (4.1%) and deep infections in 3 patients (6.25%), resulting in a total infection rate similar to that reported by Mian Amjad Ali et al.
Tibia, being more susceptible to open fractures due to the thinner soft tissue coverage compared to other bones, presents a challenge in terms of infection and wound healing. We did not come across a study focusing on the outcomes of intramedullary nailing (IMN) in tibia fractures following high-velocity gunshot injuries in the literature. Khatri et al. applied internal fixation methods to tibia fractures resulting from high-velocity gunshot injuries. In a study involving 29 patients, IMN was applied to 22 patients without reaming, while the remaining 7 patients underwent fixation with plates. Bone union occurred between the 16th and 22nd weeks in 23 patients. Delayed union was observed in 5 patients (17.2%) during the six-month follow-up, and deep infection developed in 4 patients (13.7%) [19]. In our study, the rate of cases with delayed union was lower (14.7% - 5 cases). We attributed this to the use of unreamed IMN in our study. The total infection rate in our study was 17.6% (6 patients). Most of the patients in our study were poorly self- caring individuals injured in the Syrian civil war and residing in refugee camps, which we believe contributed to the increased infection rates. We reviewed a study by Esan et al. comparing primarily locked nailing and external fixation methods in open tibia fractures. The frequency of deep wound infection was 35% (external fixation) and 11.1% (locked nailing). The mean union time was 14.8 weeks for external fixation and 14.4 weeks for locked nailing, with no statistically significant difference in the meantime (t=0.133, p=0.895) [20]. This study showed that the risk of wound infection was higher when external fixation was used in the treatment of open tibia fractures compared to unreamed locked intramedullary nails. Similarly, we applied locked IMN to 34 tibia open fractures resulting from high-velocity gunshot injuries by reaming. We found the average union time to be 22 weeks in our study. We attributed the longer union time in our study to the configuration of multi- fragmented fractures resulting from high-velocity gunshot injuries and subsequent delayed weight-bearing. We observed nonunion in two patients (5.88%). We found the total infection rate to be 17.6% (6 patients). The higher infection rate in our study may be attributed to the etiology being gunshot injuries.
The optimal protocol for the treatment of open humerus fractures has not been clearly stated in the literature. Open humerus shaft fractures should be considered as a separate entity with their treatment protocol [21]. There is currently insufficient research on humerus fractures resulting from gunshot injuries treated with IMN. In a case series involving 38 humerus fractures treated with external fixation, including 35 caused by low-velocity gunshot injuries, bone union occurred between 12 and 24 weeks (average 16 weeks). Two patients required bone grafting due to delayed union. Nonunion occurred in two patients (5%). Five patients had superficial nail tract infections, two had deep wound infections, and one had bone infection [22]. We applied locked intramedullary nails to 7 humerus shaft fractures resulting from gunshot injuries. The average union time was 10.1 weeks. We observed no cases of nonunion. One patient (14%) developed a superficial infection, which resolved after debridement and antibiotic therapy. There were no cases of deep infection or nonunion. Operating on all our patients within the first 8 hours may have reduced the infection rate. We attribute our shorter union times and achieving union in all patients to the low infection rates and the use of intramedullary nails.
Figures
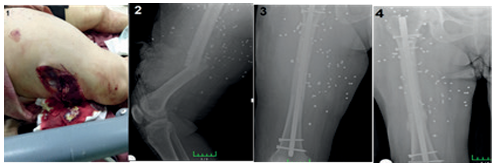
Figure 1. (1)Femur Fracture - Preoperative Radiograph (2) Postoperative Radiograph of Femoral Intramedullary Nailing (3) Type 3C Femur Fracture with Vascular Injury
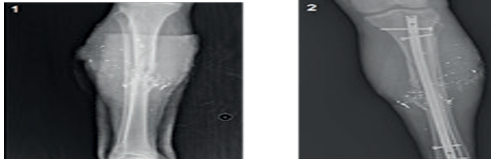
Figure 2. (1); Tibial Fracture - Preoperative Radiograph (2); Postoperative Radiograph of Tibial Intramedullary Nailing
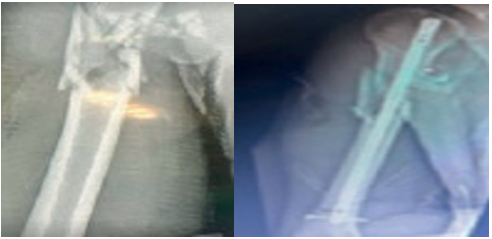
Figure 3. Humerus Fracture - Preoperative Radiograph - Postoperative Radiograph of Humerus Intramedullary Nailing
Tables
Table 1. Complications of femur interlocking nail
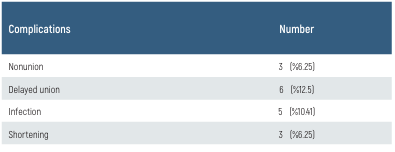
Table 2. Complications of tibia interlocking nail
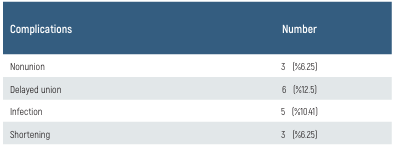
Table 3. Complications of humerus interlocking nail
Limitations
We consider the limited number of humerus fracture cases in our study as one of its limitations. Given our limited case count, reaching a definitive conclusion and making strong recommendations supporting IMN in cases of high-velocity gunshot injuries to the femur, tibia, and humerus is difficult. Additionally, since we only included IMN cases in our study, comparing with other methods was not possible. Furthermore, the inability to include Gustilo Anderson type 3b open fractures in our study has resulted in an evaluation deficiency. Another limitation of our study is having only one observer for radiological evaluation, digital measurements, and clinical evaluation, which increased the risk of bias.
Conclusion
Fractures of the humerus, femur, and tibia diaphysis resulting from gunshot injuries pose a challenging case for orthopedic surgeons. However, there is insufficient literature on the treatment of long-bone diaphyseal fractures caused by high-velocity firearms. Long-term follow-up studies with larger patient groups are needed in this regard. Our study will contribute to the existing literature on this topic. We believe that locked intramedullary nails can be applied with careful debridement and antibiotic therapy to the patient’s overall condition and the extent of soft tissue damage in the femur, tibia, and humerus diaphyseal fractures resulting from high-velocity gunshot injuries.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Nolan PC, McPherson J, McKeown R, Diaz H, Wilson D. The price of peace: The personal and financial cost of paramilitary punishments in Northern Ireland. Injury. 2000;31(1):41-5.
-
Bowyer GW, Rossiter ND. Management of gunshot wounds of the limbs. J Bone Joint Surg Br. 1997;79(6):1031-6.
-
Howland WS, Jr., Ritchey SJ. Gunshot fractures in civilian practice. An evaluation of the results of limited surgical treatment. J Bone Joint Surg Am. 1971;53(1):47-55.
-
Arslan H, Kapukaya A, Necmioglu S, Erdem H, Yildirim K. Treatment of subtrochanteric femoral fractures due to high-velocity gunshot injury. Acta Orthop et Traumatol Turc. 1997;31(2):101-5.
-
Arslan H, Subasi M, Kesemenli C, Kapukaya A, Necmioğlu S, Kayikçi C. Problem fractures associated with gunshot wounds in children. Injury. 2002;33(9):743-9.
-
Klemm KW, Börner M. Interlocking nailing of complex fractures of the femur and tibia. Clin Orthop Relat Res. 1986(212):89-100.
-
Tornetta P, 3rd, Ritz G, Kantor A. Femoral torsion after interlocked nailing of unstable femoral fractures. J Trauma. 1995;38(2):213-9.
-
Lerner A, Fodor L, Soudry M. Is staged external fixation a valuable strategy for war injuries to the limbs? Clin Orthop Relat Res. 2006;448:217-24.
-
Lavine LS, Grodzinsky AJ. Electrical stimulation of repair of bone. J Bone Joint Surg Am. 1987;69(4):626-30.
-
Nicholas RM, McCoy GF. Immediate intramedullary nailing of femoral shaft fractures due to gunshots. Injury. 1995;26(4):257-9.
-
Bergman M, Tornetta P, Kerina M, Sandhu H, Simon G, Deysine G, et al. Femur fractures caused by gunshots: treatment by immediate reamed intramedullary nailing. J Trauma. 1993;34(6):783-5.
-
Hilton T, Kruger N, Wiese K, Martin C, Maqungo S. Gunshot tibia fractures treated with intramedullary nailing: A single centre retrospective review. SA Orthopaedic Journal. 2017;16(1):32-8.
-
Brav EA. Further evaluation of the use of intramedullary nailing in the treatment of gunshot fractures of the extremities. J Bone Joint Surg Am. 1957;39-a(3):513-20.
-
Carr CR, Turnipseed D. Experiences with intramedullary fixation of compound femoral fractures in war wounds. J Bone Joint Surg Am. 1953;35-a(1):153-71.
-
Atesalp AS, Yildiz C, Başbozkurt M, Gür E. Treatment of type IIIa open fractures with Ilizarov fixation and delayed primary closure in high-velocity gunshot wounds. Mil Med. 2002;167(1):56-62.
-
Ali MA, Hussain SA, Khan MS. Evaluation of results of interlocking nails in femur fractures due to high velocity gunshot injuries. J Ayub Med Coll Abbottabad. 2008;20(1):16-9.
-
Hollmann MW, Horowitz M. Femoral fractures secondary to low velocity missiles: treatment with delayed intramedullary fixation. J Orthop Trauma. 1990;4(1):64-9.
-
Tornetta P, 3rd, Tiburzi D. Anterograde interlocked nailing of distal femoral fractures after gunshot wounds. J Orthop Trauma. 1994;8(3):220-7.
-
Khatri JP, Kumar M, Singh CM. Primary internal fixation in open fractures of tibia following high-velocity gunshot wounds: a single-centre experience. Int Orthop. 2020;44(4):685-91.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Mustafa Kemal University (Date: 2020- 11-12, No: 19)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Namık Kemal Kılınçcıoğlu, Volkan Kızılkaya, Mehmet Menken, Vedat Uruc, Yunus Dogramacı. Intramedullary nailing outcomes in open fractures due to firearm injuries. Eu Clin Anal Med 2025;13(2):40-44
Publication History
- Received:
- March 17, 2025
- Accepted:
- April 24, 2025
- Published Online:
- April 30, 2025
- Printed:
- May 1, 2025
