An investigation of medical school students’ level of knowledge on breast cancer and their attitudes toward breast self-examination
Level of knowledge on breast cancer
Authors
Abstract
Aim This study aimed to investigate the medical students’ level of knowledge about breast cancer and review their attitudes toward breast self-examination (BSE).
Material and Methods The study was performed with students studying at Kocaeli University Faculty of Medicine between January and March 2024. The study population consisted of all registered medical faculty students of that time. The questionnaire form was developed upon literature review and the final version included 31 multiple choice and direct text response items and was completed by 1st–6th grade students.
Results 443 participants who responded to the entire questionnaire, were involved in the study. There were 71 Grade 1 (16%), 72 Grade 2 (16.3%), 79 Grade 3 (17.8%), 75 Grade 4 (16.9%), 78 Grade 5 (17.6%), and 68 Grade 6 (15.3%) students in the study. The rate of those who responded that they were informed about breast cancer was 86.7% (n = 384). The rate of correct answers to the items measuring the level of knowledge was higher among the participants, who responded that they had knowledge than the others. (p < 0.001) The rate of being knowledgeable grew with each year of education during the first three years. (p < 0.001) The sources of information were medical documents 54.4% (n = 241), healthcare professionals 21.2% (n = 94), social environment 16% (n = 71), and visual media 8.4% (n = 37). The usage of medical documents increased with each year of education, reaching its highest in the 6th year with a rate of 77.9%. (p < 0.001) The rate of correct answers to the items, which measured the level of knowledge increased by the years in education, especially during the first 3 years. (p < 0.001) Again, the rate of correct answers to these items was higher in those, who used medical documents as a source. (p < 0.001)
Discussion As a result of the study, it was concluded that breast cancer awareness, level of knowledge, and the rate of those practicing BSE elevated with the number of years in education. Nevertheless, the level of knowledge and awareness about breast cancer should be higher in medical schools, which provide medical education to prospective doctors, who will constitute the basis of health care.
Keywords
Introduction
Breast cancer is the predominant cancer found in women across the world, affecting more than 2 million women each year. Among women in the United States, breast cancer is the most prevalent non-skin cancer and the second leading cause of cancer mortality [1]. In Turkey, breast cancer was reported to be the cause of approximately 4.300 women’s deaths in 2019. One out of every four women diagnosed with cancer, with a gradually decreasing age of onset, experiences breast cancer. [2] Follow-up and treatment are very important due to its high prevalence and the fact that it is associated with serious morbidity and mortality. Especially thanks to screening methods, the number of early-diagnosed patients is increasing. Consequently, providing correct information and education about breast cancer is crucial for society to adapt to the screening methods. It is very important that healthcare professionals, especially the doctors, with whom society directly deals in terms of healthcare, receive the most accurate education and have the most accurate information about breast cancer. This study aimed to raise breast cancer awareness among medical students while evaluating the differences across grades by comparing the students’ knowledge and attitudes based on their educational years.
Materials and Methods
This survey was performed with the Kocaeli University Faculty of Medicine students between January and March 2024. Prior to the study’s commencement, approval from the local ethics committee was granted. The population of the study consisted of Grade 1 to 6 students (n = 460) studying at Kocaeli University Faculty of Medicine. Participants joined the study voluntarily and were not compensated. All participants gave their informed consent. Students, who did not want to participate and were not in attendance in the classroom at that time, were not included in the study. A questionnaire consisting of 30 items with multiple choice and direct text answers was developed by two general surgeons in light of the recent literature. The first 5 items asked about the characteristics of the participants, including age, class, and marital status. The remaining 25 items were directly aimed at measuring breast cancer awareness and knowledge. The questions are as follows:
1. Do you know anything about breast cancer? (Yes/No/I don’t know) (Y/N/DN)
2. Breast cancer is the most common cancer in women. (True/False/I don’t know) (T/F/DN)
3. Breast cancer is a disease that only affects women. (T/F/DN)
4. Breast cancer is a cancer that can be seen under the age of 40. (T/F/DN)
5. Breast cancer is a cancer that can often be genetically inherited. (T/F/DN)
6. Not having children has an impact on breast cancer development. (T/F/DN)
7. Age at first childbirth over 30 years has an impact on the development of breast cancer. (T/F/DN)
8. Breast cancer is a cancer with high mortality. (T/F/DN)
9. A lump in the breast or armpit may be a sign of breast cancer. (T/F/ DN)
10. Bleeding or discharge from the nipple may be a sign of breast cancer. (T/F/DN)
11. Breast shrinkage may be a sign of breast cancer. (T/F/DN)
12. Rash on and around the nipple may be a sign of breast cancer. (T/F/ DN)
13. Change in breast size may be a sign of breast cancer. (T/F/DN)
14. Change in breast shape may be a sign of breast cancer. (T/F/DN)
15. Family history of breast cancer increases breast cancer risk. (T/F/DN)
16. Smoking increases the risk of breast cancer. (T/F/DN)
17. A body mass index greater than 25 (obesity) increases the risk of breast cancer. (T/F/DN)
18. Early menstruation increases breast cancer risk. (T/F/DN)
19. Age at first pregnancy >30 years increases breast cancer risk. (T/F/ DN)
20. Late menopausal age increases breast cancer risk. (T/F/DN)
21. Advanced age increases breast cancer risk. (T/F/DN)
22. Do you know how to do a breast self-examination? (Y/N/DN)
23. Do you perform breast self-examination? (Y/N/DN)
24. Do you think a doctor should be consulted when you notice a difference in breast self-examination? (Y/N/DN)
25. Hormone therapy has a place in breast cancer treatment. (T/F/DN)
26. Chemotherapy and radiotherapy can be applied before or after surgery in breast cancer treatment. (T/F/DN)
27. Axillary lymph node involvement in breast cancer is considered advanced stage and cannot be treated. (T/F/DN)
28. Patients who undergo surgical treatment for breast cancer do not need chemotherapy, radiotherapy, or hormone therapy. (T/F/DN)
29. After surgical treatment of breast cancer, there is a risk of recurrence in the same or opposite breast. (T/F/DN)
30. The only surgical treatment for breast cancer is mastectomy (removal of the entire breast). (T/F/DN)
The questionnaire form was physically distributed to Grade 1–6 students in the classroom environment. Those, who gave incomplete responses to the survey items were excluded from the study.
For the analysis, The Statistical Package for the Social Sciences (SPSS), Version 22.0 (SPSS Inc., Chicago, IL, USA) was utilized. The relationship or differences between groups by categorical variables were analyzed using Chi-squared and Fisher Extract tests. A p-value of < 0.05 was considered statistically significant.
Ethical Approval
This study was approved by the Kocaeli University Non-Interventional Clinical Research Ethics Committee (Date: 2024-04-25, No: KÜ GOKAEK-2024/07.27)
Results
A total of 460 students participated in the study, including 74 Grade 1, 75 Grade 2, 82 Grade 3, 78 Grade 4, 81 Grade 5, and 70 Grade 6 students. Seventeen participants with incomplete responses to the questionnaire were excluded from the study. The study was completed with a total of 443 students. 401 (90.5%) of the participants were aged between 17–24 years and 42 (9.5%) between 25–35 years. Of the participants, 438 (98.9%) were single and 5 (1.1%) were married. In the end, the participants distribution included 71 Grade 1 (16%), 72 Grade 2 (16.3%), 79 Grade 3 (17.8%), 75 Grade 4 (16.9%), 78 Grade 5 (17.6%), and 68 Grade 6 (15.3%) students.
Not a single participant had a history of breast cancer diagnosis. The percentage of participants who had relatives or persons from their social environment diagnosed with breast cancer was 37% (n = 164). The number of participants who responded affirmatively that they were informed about breast cancer was 86.7% (n = 384). Sources of information were medical documents 54.4% (n = 241), healthcare professionals 21.2% (n = 94), social environment 16% (n = 71), and visual media 8.4% (n = 37). Details on the general distribution of the answers to the items are given in Table 1.
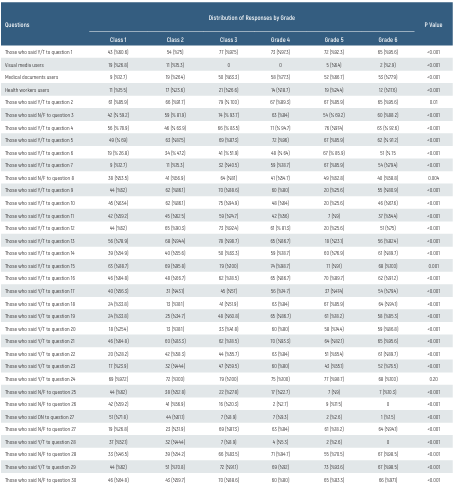
The answers to the items as categorized by years in education are given in detail in Table 2. The participants, who responded that they were informed about breast cancer were the lowest at year 1 with 60.6%, and the highest at year 3 with 97.5%. In the first three years, the rate of being knowledgeable increased significantly by years in education (p < 0.001). While the use of visual media as a source of information was the highest in year 1 with 26.8%, this rate gradually decreased in the following years. The use of medical documents increased with years of education and reached its highest in year 6 with 77.9%. (p < 0.001) The number of participants, who chose healthcare professionals as their source of information, was lowest in year 1. (p < 0.001) The rate of affirmative and/or correct responses to the items below grew with each year of education, especially during the first 3 years (p < 0.001): “Breast cancer is the most prevalent cancer in women,” “Only women are affected by breast cancer,” “Not having children has a role in the onset of breast cancer,” “The age of first childbirth over 30 has an effect on the development of breast cancer.”, “Breast cancer is associated with high mortality.”, “Is a lump in the armpit and breast a sign of breast cancer?”, “Is bleeding or discharge from the nipple a sign of breast cancer?”, “Is shrinkage in the breast a sign of breast cancer?”, “Is a rash on and around the nipple a sign of breast cancer?”, “Is a change in breast size a sign of breast cancer? “ “Is a change in breast shape a sign of breast cancer?”, “Breast cancer risk is increased by a family history of the disease.”, and “Do you perform breast self-examination?”. The answers of the participants who responded they were and were not knowledgeable are given in detail in Table 3. The rate of affirmative and/or correct responses to the items below was significantly higher among the participants, who reported that they were knowledgeable (p < 0.001): “Breast cancer is the most prevalent cancer in women.”, “Breast cancer is only seen in women.”, “Not having children has an effect on the development of breast cancer.”, “The age of first childbirth over 30 has a role in the onset of breast cancer.”, “Breast cancer is associated with high mortality.”, “Is a change in breast shape a sign of breast cancer?”, “A familial history of breast cancer increases the risk of breast cancer.”, “Do you perform breast self-examination, do you know how to do it?”, “Does early menstruation increase the risk of breast cancer?”, “Does age at first pregnancy >30 years increase the risk of breast cancer?”, “Does late menopausal age increase the risk of breast cancer?”, “Is there a risk of recurrence in the same or opposite breast after surgical treatment of breast cancer?”, “Can chemotherapy and radiotherapy be applied before or after surgery in breast cancer treatment?”, and “Chemotherapy, radiotherapy or hormone therapy are unnecessary for patients who undergo surgical treatment for breast cancer.”
An overview of the participants’ responses by the sources from which they obtained information is given in detail in Table 4. The rate of affirmative and/or correct responses to the below items was significantly higher in those, who used medical documents as a source (p < 0.001): “Breast cancer is the most prevalent cancer in women”, “Breast cancer is only seen in women”, “Not having children has an effect on the development of breast cancer”, “The age of first childbirth over 30 has an effect on the development of breast cancer”, “Is a change in breast shape a sign of breast cancer?”, “A familial history of breast cancer increases the risk of breast cancer”, “Does smoking and alcohol consumption increase the risk of breast cancer?”, “Does an elevated body mass index (greater than 25) raise the risk of breast cancer?”, “Do you perform breast self-examination?”, “Does early menstruation increase the risk of breast cancer?”, “Does age at first pregnancy >30 years increase the risk of breast cancer?”, “Does late menopausal age increase the risk of breast cancer?”, “Does advanced age increase the risk of breast cancer?”, “Is there a risk of recurrence in the same or opposite breast after surgical treatment of breast cancer?”, and “Can chemotherapy and radiotherapy be applied before or after surgery in the treatment of breast cancer?”.
The rate of affirmative and/or correct responses to the below items was significantly higher in those, who received information from healthcare professionals (p < 0.001): “Breast cancer is cancer that can often be genetically transmitted”, “Do you know how to perform breast self-examination?”, and “Patients, who undergo surgical treatment for breast cancer do not need chemotherapy, radiotherapy or hormone therapy treatments”.
The rate of affirmative and/or correct responses to the below items was significantly higher in those, who used visual media as a source of information (p < 0.001): “Breast cancer is a cancer with high mortality” and “Can a change in breast size be a sign of breast cancer?”.
Discussion
Breast cancer is the predominant cancer found in women. The most important instrument in developing protective behaviors against such a common cancer is to raise awareness by increasing people’s knowledge about breast cancer. Awareness and education about breast cancer is crucial for early diagnosis. Accordingly, it can be ensured that both breast self-examination (BSE) as recommended by the World Health Organization is widely adopted and participation in screening programs is increased. (http://apps.who.int/iris/bitstream/ handle/10665/254500/9789241511940) Without a doubt, the main providers of this training are healthcare professionals, and especially the doctors. This study was designed to assess the effect of the education received by prospective medical students on breast cancer awareness and knowledge level over the years. In a study conducted among all university students in Pakistan, it was found that students had very little knowledge involving the risk factors, signs, and symptoms of breast cancer and breast examination. [3] In a study conducted among high school and university students, it was reported that breast cancer awareness was insufficient. [4] In a study conducted among medical students, it was found that breast cancer awareness was quite deficient. [5] In another study, it was reported that although medical students’ knowledge about breast cancer risk factors was significantly better than non-medical students, it was generally inadequate. [6] A separate study indicated that the level of breast cancer awareness was similar between medical faculty students and non-medical faculty students. [7] In a study conducted in another center, it was reported that the level of breast cancer knowledge was low among university students and moderate among medical students. [8] In a previous similar study, the most frequent source of information for medical students was school/faculty with 61.8%. [9] Another study reported this rate as 39.2%. [10] In the present study, the medical documentation was the primary source for students can obtain information with 54.4% (n = 241). This was indicative of the fact that medical students tried to obtain information from scientific and more accurate sources. It was seen that a high rate of correct responses was given in items, where basic knowledge was questioned (e.g., breast cancer is the most prevalent cancer in women, it can be seen under the age of 40, and it is only seen in women). Nevertheless, the rate of correct answers decreased significantly in items that asked about risk factors or more advanced knowledge about treatment issues. This was suggestive of the fact that the available education was somehow superficial and that more inclusive training was required. A previous study with medical school students reported that the rate of those, who performed BSE, was 42.9%. [10] Another study found this rate as 33.5%. [9] A study with nursing students reported this rate as 63%. [11] In another study with female healthcare workers, this rate was 22%. [12] A study with midwifery students reported this rate as 84.9%. [13] In the present study, the rate of students, who performed BSE was 56.7%. This rate can be considered low for medical students. No variation in knowledge levels was observed between the clinical and pre-clinical stages. [14] But in our study, the rate of those, who responded that they were knowledgeable about breast cancer increased years in education, especially during the first three years. Were the participants, who said they were informed, really informed? Upon analysis of the responses to the items, which measured the participants’ level of knowledge in order to answer the above question, it was seen that the majority of the items (79.2%) were answered with a higher accuracy rate by the participants, who responded that they were knowledgeable. The findings also indicated that the correct answer rate improved as the participants’ years in education increased (especially during the first 3 years) for the majority of the items, which measured the level of knowledge (68.6%). The rate of those, who performed BSE also increased by years in education. This is indicative of the effect of the level of education on breast cancer awareness, knowledge level, and practice of BSE. We believe that better education may help increase these rates for the prospective doctor. The use of visual media as a source of information was highest in Grade 1, which gradually decreased. The use of medical documentation increased by years in education and reached its highest level in Grade 6 Upon an analysis of the responses to the items, which measured the level of knowledge, it was seen that the participants, who used medical documentation as a source, gave more correct answers in most of the items (56.7%) compared to those, who used other sources. This was indicative of the fact that as the number of years in education increased, participants turned to sources that led to more scientifically valid and accurate information, which was beneficial in increasing the level of knowledge. Facilitating and promoting access to medical sources of scientific and accurate information will further improve the quality of education. As stated in previous studies, it can be said that more effective health education programs are needed. [15] This will have positive consequences for the public in terms of breast cancer awareness.
The study’s main limitation is that the questionnaire was administered only to students from one single medical school. As a result, the findings of this study cannot be broadly applied to all medical students. More general conclusions can be reached with future studies involving other medical schools with wider participation.
Tables
Table 1. General Distribution of Responses to the Questions

Table 2. Distribution of Responses to the Questions According to Classes
Limitations
The study is primarily limited by its retrospective nature and the small sample size.
Conclusion
In conclusion, early diagnosis is very important in the fight against breast cancer and the most important way to early diagnosis is undoubtedly the screening methods. The education of individuals is of great importance in terms of guiding all segments of society, including healthcare professionals, to these methods. Quality of education increases through the use of medical documentation as a source of information in educational activities. As a result of the study with medical students, it was concluded that breast cancer awareness, level of knowledge, and the rate of those practicing BSE increased by years in education. Furthermore, the level of knowledge and awareness about breast cancer should be higher from the first grade in medical schools, which provide education to prospective doctors, who form the basis of health care. Therefore, breast cancer awareness can be raised through organizations, including conferences, courses, etc. within the education process.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics. CA Cancer J Clin. 2023;73(1):17-48.
-
Doğan N, Doğan İ, Toprak D. Geographical distribution and trends of women breast cancer mortality in turkey between 2009-2019. Ank Med J. 2023;23(4):366-77.
-
Hussain I, Majeed A, Masood I, Ashraf W, Imran I, Saeed H, et al. A national survey to assess breast cancer awareness among the female university students of Pakistan. PLoS One. 2022;17(1):e0262030.
-
Mafuvadze B, Manguvo A, He J, Whitney SD, Hyder SM. Breast cancer knowledge and awareness among high school and college students in mid-western USA. Int J Sci Educ. 2013;3(2):144-58.
-
Omar A, Bakr A, Ibrahim N. Female medical students’ awareness, attitudes, and knowledge about early detection of breast cancer in Syrian Private University, Syria. Heliyon. 2020;6(4):e03819.
-
Noreen M, Murad S, Furqan M, Sultan A, Bloodsworth P. Knowledge and awareness about breast cancer and its early symptoms among medical and non-medical students of Southern Punjab, Pakistan. Asian Pac J Cancer Prev. 2015;16(3):979-84.
-
Mohamed EY, Sami W, Alenezi AA, Almutairi AM, Alsalboud AK, Alhusainy KM et al. Breast cancer awareness and breast self-examination among future female university graduates: comparison between medical and non-medical students. Int J Res Med Sci. 2016;4(3):685-89.
-
Akter MF, Ullah MO. Awareness levels of breast cancer among female university and medical college students in Sylhet city of Bangladesh. Cancer Rep (Hoboken). 2022;5(11):e1608.
-
Düzova M, Yiğit Nİ, Esen FZ, Akman NB, Türkyilmaz FN, Atci AA, et al. Breast self-examination and breast cancer awareness in medical students: A survey study in a medical school. J Gen Med. 2023;33(1):82-86.
-
Yılmaz S, Nilüfer E, Aykota MR. Evaluation of medical students’ knowledge and attitudes about breast cancer and breast self-examination. Pamukkale Med J. 2020;13(2):351-56.
-
Aslan A, Temiz M, Yiğit Y, Can R, Canbolant E, Yiğit F. Knowledge, attitudes and behaviors of School of Nursing students about breast cancer. TAF Prev Med Bull. 2007;6:193-8.
-
Özçam H, Çimen G, Uzunçakmak C, Aydın S, Özcan T, Boran B. Evaluation of knowledge, attitudes and behaviors of female health workers regarding breast cancer, cervical cancer and routine screening tests. Ist Med J. 2014;15(3):154-60.
-
Aytekin MŞ, Çetin Ö, Kahraman A. Determination of the relationship between breast self- examination and fear of breast cancer in midwifery students and their mothers. Anatol J Health Res. 2022;2(3):93-100.
-
Balakrishnan P, Kodamanchili SPDR, Kumar AA, Raju K, Gabunia L. Breast cancer awareness among medical students in Georgia. Inte J Prog Sci Tech. 2022;33(1):58-73.
-
Joy N, D’Souza C, D’Souza CR. Breast cancer awareness among undergraduate medical students in a tertiary healthcare centre in Mangalore, India. Int Surg J. 2018;5(12):3842-46.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Kocaeli University Non-Interventional Clinical Research (Date: 2024-04-25, No: KÜ GOKAEK-2024/07.27)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Enes Şahin, Mehmet Eşref Ulutaş, Sümeyye Şahin, Kazım Şahin, Dila Önal, Sertaç Ata Güler, Nihat Zafer Utkan. An investigation of medical school students’ level of knowledge on breast cancer and their attitudes toward breast self-examination. Eu Clin Anal Med 2024;12(3):36-40
Publication History
- Received:
- August 2, 2024
- Accepted:
- August 29, 2024
- Published Online:
- August 31, 2024
- Printed:
- September 1, 2024
