Enhancing ankle and foot reconstruction: Outcomes and techniques with sural flaps in diverse patient groups
Sural flap techniques in ankle and foot reconstruction
Authors
Abstract
Aim This study aims to describe our experiences with the use of sural flaps in the reconstruction of ankle and surrounding tissue losses in different patient groups and the methods used to ensure the safety of the flap pedicle.
Material and Methods Data of 25 patients including 13 women and 12 men, who were operated between 2018 and 2023, were retrospectively analyzed. Ages ranged between 12 and 71 (mean: 42.2 years).
Results The wound and defect etiology were trauma in 9 patients, tumoral mass excision in 2 patients, chronic wound in 5 patients, diabetes in 7 patients, and lumbar disc hernia related neuropathy in 2 patients. Tissue loss was present in and around the heel in 13 patients, lateral foot in 4 patients, and around the ankle in 8 patients. In the 17 patients, sural flap procedures were performed from the identical legs. In the 8 patients were harvested sural flap from the opposite legs as cross leg flaps. Nearly in all of the patients were experienced to partial loss in the grafts, because it could have not applied pressure to the area on the flap pedicle. But this condition did not cause any healing problems in the flaps. Only in 4 patients developed complication. But it was healed with antibiotic-therapy and local wound care.
Discussion We believe that passage of the flap pedicle through open skin tunnel and closure with skin graft only, would avoid the negative effect formed by the pressure, and increase the success of the flap.
Keywords
Introduction
Correction of soft tissue loss around the distal tibia and ankle is difficult. Vascular network of that site is weak and indistinct in terms of flap surgery. Diabetes, vascular failure, neuropathy and severe traumas make the reconstruction of the site even more difficult [1, 2]. To date, many reconstruction methods have been used in ankle and heel defects with the bony structures and tendons left open. These include skin grafts, cutaneous-fasciacutaneous local flaps, muscle flaps and free tissue transplantations [3, 4, 5]. Each technique has its own advantages and disadvantages. Among these, “reverse-flow sural flaps” (will be mentioned as “sural flap” in the text) were first defined by Masquelet et al [6]. Sural flaps are being used in the reconstruction of ankle and surroundings with many modifications since then [7, 8, 9]. The close relation between the blood circulation of the flap and the venous system increases the importance of protection of the flap pedicle against pressure especially in terms of venous drainage [10, 11].
The present study describes our experiences about the usage of sural flaps in the reconstruction of tissue losses in the ankle and surroundings and about the methods used for providing safety of flap pedicle in different patient groups.
Materials and Methods
Participants
Data of 25 patients including 13 women and 12 men, who were operated between 2018 and 2023 in department of plastic reconstructive and aesthetic surgery. Data regarding clinicopathologic characteristics and treatment details were retrospectively collected. The surgery plans for all patients were formulated in accordance with institutional guidelines.
Surgical procedure
All the patients were performed tourniquet. The flap with a proper size for the defect was planned to place in the middle of the two heads of the gastrocnemius muscle. Following the skin incision surrounding the flap, fascia profunda was accessed, sural nerve and small saphenous vein were preserved on the proximal side and fastened and cut. The skin over the flap pedicle was subcutaneously opened via zig-zag incision towards the lateral malleolus. Flap pedicle was then lifted via a fat pad with a 4 cm size in order to obtain more collateral veins and facilitation of venous return. The pedicle was lifted sub-dermally in the superficial plan and adipofascially including deep fascia and excluding the skin in the deep plan. The flaps were lifted cutaneous venoneuroadipofascially including the small saphenous vein, sural nerve and median sural artery. Flaps were lifted up from the deep tissue until 6 cm proximal to the lateral epicondyle where the septocutaneous perforating branches of the peroneal artery were anastomosing with median superficial sural artery. The flap was rotated at that point in order to obtain a channel of the skin, and through that channel, the pedicle was rotated and adapted to the host site. Then the surface of the adipofascial flap pedicle was closed via a partially thick skin graft. The skin defects within the flap donor site were all closed via partially thick skin grafts except one patient. The patients were kept in the prone position for five days in order to eliminate the risk of pressure against the flap or the pedicle. In the following two weeks, the patients were allowed to lay how they desired with the restriction of any pressure to the flap pedicle. No splint was used and no external suction drain was placed in the surgery site for none of the patients. No venous congestion was observed.
Statistical analysis
Statistical analysis was performed by using statistical package for the social sciences version 27 (SPSS Inc; Chicago, IL, USA). Descriptive data were given as mean and standard deviation (SD) for quantitative variables in frequencies, and percent for qualitative variables.
Ethical Approval
The study was initiated after the approval of Mustafa Kemal University Ethics Committee (Date: 2015-05-07, No: 2015-07/5).
Results
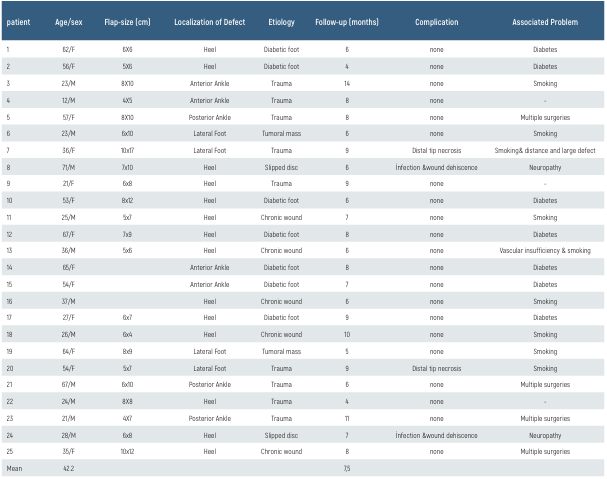
Ages ranged between 12 and 71 (mean: 42.2 years). The wound and defect etiology were trauma in 9 patients, tumoral mass excision in 2 patient, chronic wound in 5 patients, diabetes in 7 patients, and lumbar disc hernia related neuropathy in 2 patients. Tissue loss was present in and around the heel in 13 patients, lateral foot in 4 patients, around the ankle in 8 patients (Table 1). In the 17 patients, sural flap procedures were performed from the identical legs (Figure 1A-B). In the other 8 patients were harvested sural flap from the opposite legs as cross leg flaps (Figure 1C-E).
The procedures and results of some patients’ surgical operations are shown in Figure 2 and 3.
Nearly in all of the patients were experienced to partial loss in the grafts, because it could have not applied pressure to the area on the flap pedicle. But this condition did not cause any healing problems in the flaps. Only in 4 patients developed complication. In the two patients, flap was lifted 3 cm over the popliteal crease, and a necrosis band of approximately 2 cm size was observed. However, the necrotic band was excised successfully and the defect was primary closed. In the other two patients emerged infection. But it was healed with antibiotic therapy and local wound care.
Discussion
It is difficult to repair the cutaneous and subcutaneous tissue losses of the foot and ankle region. Because, the surrounding tissue is limited and weak. Furthermore, the blood support of the local flaps in this region is usually weak and indistinct. Thus, free flaps anastomosed to large vessel pedicles are used in the repair of these defects [4, 5]. Free flap applications are usually difficult since it takes a long time to place them; it necessitates special equipment and experienced specially trained surgeons [4, 5, 12, 13]. Success rates are low in especially the diseases that cause circulatory insufficiency [14]. In certain situations, such as damaging of the main vessels, usage of large arteries as host vessels may be risky for the extremity in the region under circulatory danger. Furthermore, some patients may not be proper for long-term anesthesia. Therefore, local flaps placed with conventional surgical instruments, have been used as safe alternative options with low donor-host morbidity rates and short surgical time. Various fascial- fascia cutaneous and distal flow muscle flaps have been used to repair the tissue defects of the ankle and surrounding tissues [15, 16]. However, the weak and unreliable rotational arcs and blood circulation of the local flaps, and improper wound closure with insufficient thickness are the disadvantages of these flaps. Functional loss in motor functions and bulky formation are the undesired functional and cosmetic disadvantages of the muscle flaps. Sural flaps which were first defined by Masquelet et al. [6] on the other hand, have a reliable rotational arc and may thus be used safely in the closure of 1/3 distal crural region and foot defects.
Sural flap skin island is fed in a retrograde manner by the anastomosis network formed by the perforating branches of the comitant arteries of the small saphenous vein and peroneal artery in the level of lateral malleolus, and the median superficial sural artery. And the venous drainage is supplied by the veins of the comitant arteries of the small saphenous vein [9, 17]. Theoretically for the sural flap which is planned to have a reverse flow, although a venous congestion risk is present since the flow is provided opposite to the route of the valves in the small saphenous vein, usually no problem is met in the venous drainage.
Because the small saphenous vein is thrombosed just after the surgery and no contribution to the drainage of the flap has been shown [13, 18]. The long pedicle size of the sural flap, the close relation of the blood circulation with the venous system, the retroverted flow, and the thin structures of the arteries and veins make the circulation of the flap sensitive. Thus, any pressure that the pedicle may meet negatively affects the viability of the flap. It has been observed in a wide series of studies that the highest risk group in reverse-flow sural flap surgery includes patients with venous failure [19]. In the systematic review study of Catherine de Blacam et al. on 907 patients with defect closure with sural flap including various study groups, the general complication risk was found to be 26.4% [19]. Factors such as gender, procedure, diabetes, hypertension, smoking, neurologic disease and peripheral vascular disease were found not to be related to the observation of complications. However, venous failure and age were found to be related to the complications. As complications, venous congestion is the most frequent with a rate of 2.6 % after total or partial flap loss (18.5 %) [19]. In order to avoid venous congestion, Tan et al. have anastomosed the proximal end of the small saphenous vein to one of the neighboring veins as a super charge, after the adaption of the flap to the host area [20]. In another study, the subcutaneous tunnel was opened wide in order to provide the safety of the flap pedicle. In this study with a mean age of 28.4 patients with chronic diseases such as arterial hypertension, diabetes, peripheral vascular disease and vasculitis were excluded. However, partial necrosis was still reported in 16% of the patients [21]. We believe that the pedicle passed through the subcutaneous tunnel may carry the risk of compression as a result of the oedema and inflammation observed in time. This risk may even be higher in the elderly and in patients with vascular failure.
In our study, sural flap pedicles were lifted adipofascially without skin, and passed through the open cutaneous tunnel. Flap pedicle is completely closed with partially thick skin graft. Therefore, we believe that the pressure on the flap has been reduced and venous return has been facilitated. The mean age in our study was around 42 years and our study did not include selected patients. It included patients with diabetes, neuropathy, traumas and venous failure, and those who were smoking. We experienced a partial circulatory problem in only one patient. We think that it is because we exceed the vascular territorial field [22].
In the comparative study of Kristoffer et al. on 27 patients, adipofascial lifting of the flap excising from the skin and subcutaneous fat tissue was compared to the lifting of the pedicle and flap island together with the skin, and venous congestion complication was reported to significantly decrease [23]. On the other hand, there are studies indicating increased flap viability with pre-operative delay [10, 19]. In the wide series review of Catherine de Blacam, similar complication rates were reported from patients with and without delay (26.4% vs 26.7%) [19].
We believe that adipofascial lifting of the sural flap pedicle is safer. Since the passage through the sub-dermal tunnel may increase the pressure, passage through the open skin tunnel may avoid the risk of pressure on the pedicle [24, 25]. Passage of the adipofascial lifted flap pedicle through the open skin tunnel and over grafting will avoid a second operation where the pedicle lifted together with the skin is needed to be returned back. Lifting the flap island with the skin will provide safe filling of the defect areas with a tissue volume of sufficient thickness.
Figures

Figure 1. 53-year-old women with diabetic wound. (A) In the patient was harvested sural flap from the identical leg and flap pedicle covered by skin graft. (B) The view of case at 3 months after the operation that needs a debulking procedure. (C) A 23-year-old man was harvested sural flap from the opposite legs. Because the leg had not sufficiently tissue around the defect that exposed the tibia. The flap pedicle was covered by skin graft totally. (D, E) Final results at 18 months.

Figure 2. A 36-year-old man of whom had vascular failure after the vascular trauma. (A) The case had a chronic wound on the medial malleolus. (B) The pedicle was lifted 4 cm width in order to obtain more collateral veins. (C) Postoperative appearance with split-thickness skin grafting over remaining exposed pedicle. (D) Postoperative view on 12 days.
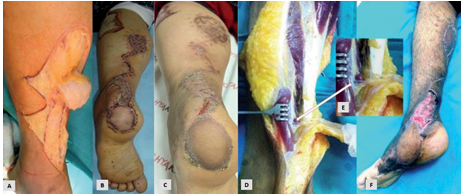
Figure 3. A 62-year-old woman with diabetic foot. (A) The pedicle was lifted sub-dermally in the superficial plan and adipofascially including deep fascia. (B) The pedicle was closed via a split thickness skin graft. (C) Final wound closure at 6 months. D-F: A 23-year-old man with a lateral foot defect from excision of the benign soft tissue tumor. (D, E) The pedicle was turned from the point of the perforator of the peroneal artery (arrow). (F) Final wound closure at 3 months.
Tables
Table 1. Patient characteristics
Limitations
Our study has certain inherent limitations that must be acknowledged. First, the retrospective design raises questions about the generalizability of our findings. Furthermore, the small sample size limits the applicability of our results, particularly within a narrowly defined group. Future research with larger sample sizes could yield more robust outcomes. While our study provides valuable insights into the right colon cancer surgery, it underscores the necessity for ongoing, extensive research to better understand the complex factors affecting patient outcomes.
Conclusion
In conclusion, easy applicability with routine surgical methods, low donor site morbidity, ability to provide a closure of sufficient thickness and applicability without risking the circulation of the foot make the sural flaps a proper option for the repair of tissue defects around the ankle. We believe that passage of the flap pedicle through the open skin tunnel and closure with a skin graft only, would avoid the negative effect formed by the pressure, and increase the success of the flap.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Cho EH, Garcia RM, Pien I, Kuchibhatla M, Levinson H, Erdmann D, et al. Vascular considerations in foot and ankle free tissue transfer: Analysis of 231 free flaps. microsurgery. 2016;36(4):276-83.
-
Govshievich A, Bauder A, Kovach SJ, Levin lS. Aesthetic considerations in extremity salvage and reconstruction. plast reconstr surg. 2023;151(4):679e-687e.
-
Antúnez M, Huyen C, Neiman R. Pedicled peroneus brevis muscle flaps as an alternative to fasciocutaneous rotational flaps for lower-extremity soft tissue defects. j orthop trauma. 2024;38(3):e105-e110.
-
Woo SJ, Park KH, Woo SH. Simultaneous or delayed free tissue transfer in combination with replantation surgery. hand clinics. 2024;40(2):301-13.
-
Yoshimatsu H, Yamamoto T, Hayashi N, Kato M, Iida T, Koshima I. Reconstruction of the ankle complex wound with a fabricated superficial circumflex iliac artery chimeric flap including the sartorius muscle: a case report. microsurgery. 2017;37(5):421-5.
-
Masquelet AC, Romana MC, Wolf G. Skin island flaps supplied by the vascular axis of the sensitive superficial nerves. plast reconstr surg. 1992;89(6):1115-21.
-
Kareh AM, Felder JM. Successful use of delayed reverse sural artery flap in single vessel legs with severe atherosclerotic disease and venous insufficiency. plast reconstr surg - global open. 2023;11(1):4740-5.
-
Park JH, Choi IC, Hong TC, Kang JW, Park JW. Reconstruction of the weight-bearing heel with nonsensate reverse sural artery flaps. injury. 2021;52(7):1993-8.
-
Schmidt K, Jakubietz MG, Gilbert F, Fenwick A, Meffert RH, Jakubietz RG. Muscle cuff in distal pedicled adipofascial sural artery flaps: A retrospective case control study. plast reconstr surg - global open. 2021;9(3):3464-9.
-
Dai J, Zhou Y, Mei S, Chen H. Application of the distally based sural neurocutaneous flaps in the management of foot and ankle defects in patients with diabetic foot. front endocrinol. 2022;13(9):1-7.
-
Huang h-h, wu z-y, chen x-f, shi y-c, xu s-h, wang s-j, et al. A modified perforator- based stepladder v-y advancement flap in the achilles tendon area for coverage of larger posterior heel defects. j plast reconstr aesthet surg. 2023;77(2):31-8.
-
Chandrasekar S, Tiwari R, Ganesan K, Singhal M. Double microvascular free flap reconstruction for bilateral lower extremity injury in a paediatric patient. bmj case rept. 2024;17(1):257181-5.
-
Mofikoya B, Ofodile N, Ogedegbe F, Akinmola O. Microvascular reconstruction for complex lower-extremity trauma in pregnancy. niger postgrad med j. 2023;30(3):258-64.
-
Akhtar S, Ahmad I, Khan AH, Khurram MF. Modalities of soft-tissue coverage in diabetic foot ulcers. adv skin wound care. 2015;28(4):157-62.
-
Bui PV, Rizzo DA. Lower limb muscle flaps. clin podiatr med surg. 2020;37(4):649-70.
-
Scaglioni MF, Meroni M, Knobe M, Fritsche E. Versatility of perforator flaps for lower extremity defect coverage: technical highlights and single center experience with 87 consecutive cases. microsurgery. 2022;42(6):548-56.
-
Xia Z, Li P, Wang Y, Wang W, Hu C, Cao X, et al. Application of 3 different types of pedicled adipofascial flaps in the repair of deep dead space wounds. wounds. 2023;35(3):47-52.
-
Alban A, Meroni M, Fuchs B, Scaglioni MF. Combined use of lower medial thigh perforator flap and pedicled medial sural artery perforator flap for lateral knee defects coverage after sarcoma resection: A case report and literature review of soft tissue defect ar. microsurgery. 2024;44(1):1-8.
-
De Blacam C, Colakoglu S, Ogunleye AA, Nguyen JT, Ibrahim AMS, Lin SJ, et al. Risk factors associated with complications in lower-extremity reconstruction with the distally based sural flap: a systematic review and pooled analysis. j plast reconstr aesthet surg. 2014;67(5):607-16.
-
Tan O, Atik B, Bekerecioglu M. Supercharged reverse-flow sural flap: a new modification increasing the reliability of the flap. microsurgery. 2005;25(1):36-43.
-
Uygur F, Evinç R, Noyan N, Duman H. should we hesitate to use subcutaneous tunneling for fear of damaging the sural flap pedicle?. Ann Plast Surg. 2009;63(1):89-93.
-
Follmar KE, Baccarani A, Baumeister SP, Levin LS, Erdmann D. The distally based sural flap. Plast Reconstr Surg. 2007;119(6):138e-148e.
-
Sugg KB, Schaub TA, Concannon MJ, Cederna PS, Brown DL. The reverse superficial sural artery flap revisited for complex lower extremity and foot reconstruction. Plast Reconstr Surg Glob Open. 2015;3(9):519-25.
-
Herlin C, Sinna R, Hamoui M, Canovas F, Captier G, Chaput B. Distal lower extremity coverage by distally based sural flaps: Methods to increase their vascular reliability. Ann Chir Plast Esthet. 2017;62(1):45-54.
-
Tsai J, Liao HT, Wang PF, Chen CT, Lin CH. Increasing the success of reverse sural flap from proximal part of posterior calf for traumatic foot and ankle reconstruction: Patient selection and surgical refinement. Microsurgery. 2013;33(5):342-9.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Mustafa Kemal University (Date: 2015- 05-07, No: 2015-07/5)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Metin Temel, Ahmet Kahraman, Numan Atilgan. Enhancing ankle and foot reconstruction: Outcomes and techniques with sural flaps in diverse patient groups. Eu Clin Anal Med 2024;12(3):50-54
Publication History
- Received:
- August 13, 2024
- Accepted:
- August 28, 2024
- Published Online:
- August 31, 2024
- Printed:
- September 1, 2024
