Evaluation of the relationship between inflammatory markers (SII, NLR, PLR, and MPV) and diagnostic parameters of 68Ga-PSMA PET/CT in prostate cancer patients?
Ga-68 PSMA PET/CT and inflammatory markers
Authors
Abstract
Aim The link between cancer and inflammation is of interest to many researchers. This study aims to determine the relationship between inflammatory parameters (SII, NLR, PLR, and MPV) and diagnostic parameters of 68Ga- PSMA PET/CT (SUVmax and HU). In addition, we aimed to compare these data with PSA values and metastasis patterns in prostate cancer patients.
Material and Methods Seventy-five prostate cancer patients who were sent to the Nuclear Medicine Department for 68Ga-PSMA PET/CT imaging, who did not undergo a undergo a prostatectomy and radiotherapy, and who had a complete blood count within a few weeks before or after imaging were included in the study. SII, NLR, PLR, and MPV were studied as inflammatory parameters. HU and SUVmax of the areas showing the highest uptake from the tumor areas in the prostate were measured from 68Ga-PSMA PET/CT.
Results Metastasis was present in 58 (77.3%) patients. Lymph node metastasis was found to be more common in patients with SII≥726 and NLR value ≥3 (p=0.007 and 0.025, respectively). According to median MPV values, patients were divided into two groups: patients with MPV values <9.5 and ≥9.5, and diffuse bone metastasis was found to be higher in patients with MPV values <9.5 (p=0.023). Also, a negative correlation was found between MPV values and PSA (p=0.008,r=-0.310).
Discussio A statistically significant relationship between high SII and high NLR values and lymph node metastasis, a negative correlation between MPV and PSA, and a relationship between low MPV values and widespread bone metastasis was found. For this reason, it should be kept in mind during clinical follow-up that PSA levels, as well as hemogram data, carry signs of possible metastasis.
Keywords
Introduction
Prostate cancer is the most frequently diagnosed cancer among men in more than half of the world’s countries and is the second most common cause of cancer-related deaths 1. In the standard treatment protocol of prostate cancer patients, prostatectomy or radiotherapy, chemotherapy, and hormonotherapy are used according to the stage of the disease. Also, recently, radionuclide treatments with Lu-177 PSMA have been used in patients with metastatic castration-resistant prostate cancer (CRPC).
Although CT (Computed Tomography), MRI (Magnetic Resonance Imaging), and bone scintigraphy are frequently used in the diagnosis of prostate cancer patients, imaging of recurrences and metastases, 68Ga-PSMA PET/CT (Positron Emission Tomography/Computed Tomography) has been used in many centers in recent years. PSMA is a type II transmembrane protein whose expression increases 100-1000 times more in prostate cancer cells. With this imaging method, both staging and detection of recurrence/metastases in prostate cancers can be made more accurate 2.
Gleason score, Eastern Cooperative Oncology Group performance status (ECOG PS), lactate dehydrogenase (LDH), prostate-specific antigen (PSA), alkaline phosphatase (ALP), location of metastases, and blood cell entities have long been recognized as potential prognostic factors in CRPC patients 3. It is known that the tumor microenvironment is very effective in determining the characterization of the tumor, and many types of cancer (renal cell carcinoma, hepatocellular carcinoma, triple- negative breast cancer, gastric cancer, and head and neck cancers) are characterized by the presence of inflammation 4. However, the role of inflammation in the development of prostate cancers has not yet been fully explained. Inflammatory infiltrates can be seen in benign pathologies such as prostatitis in the prostate gland. Studies show that inflammation weakens the anticancer therapy effectiveness 5. Based on this situation, studies on neutrophil/lymphocyte ratios (NLR) and platelet lymphocyte ratio (PLR) have been conducted to evaluate the effect of inflammation in many types of cancer 6,7,8. A new inflammatory parameter called the systemic-immune-inflammation index (SII) has recently been defined 9. According to Lolli et al. 10, SII is a strong prognostic index in prostate cancers. All three parameters can be easily calculated from routine complete blood counts from the peripheral blood.
This study aims to determine the relationship between inflammatory parameters (SII, NLR, PLR, and MPV) and diagnostic parameters of 68Ga-PSMA PET/CT (SUVmax and HU). In addition, we aimed to compare these data with PSA values and metastasis patterns in prostate cancer patients.
Materials and Methods
Patients
Patients who were sent to the Nuclear Medicine Department for 68Ga- PSMA PET/CT imaging between August 2019 and September 2020, who did not undergo a undergo a prostatectomy and radiotherapy, and who had a complete blood count within a few weeks before or after 68Ga- PSMA PET/CT imaging were included in this study. The histopathology and treatment data of the patients were obtained from the hospital information management system and patient records in our department. Patients who had previously received radiation therapy to the area of the prostate gland were not included in this study.
SII, NLR, PLR, and MPV (mean platelet volume) were studied as inflammatory parameters. The systemic-immune-inflammation index (SII) is calculated by (N×P)/L (N, P, and L represent neutrophil counts, platelet counts, and lymphocyte counts, respectively). The Neutrophil/ lymphocyte ratio (NLR) is calculated as the ratio of the neutrophil to lymphocyte count. Platelet lymphocyte ratio (PLR) is calculated as the ratio of the platelet to lymphocyte count. All variables were obtained from the same blood sample.
Hounsfield unit (HU) and SUVmax of the highest 68Ga-PSMA uptake from the tumor areas in the prostate gland were measured from 68Ga- PSMA PET/CT. In each patient, the areas of interest were measured at an equal size of mm2. Prostate volume was calculated by using a volume of an ellipsoid formula via CT images (width × depth × length x π x 4/3).
Prostate cancer metastasis patterns have been grouped as lymph node metastasis, distant organ metastasis, bone metastasis, and widespread bone metastasis.
The study had a retrospective design and informed consent was obtained from all patients. All reported investigations were conducted in accordance with the principles of the Declaration of Helsinki.
68Ga-PSMA PET/CT Imaging Protocol
Patients received an intravenous injection of 2 MBq/kg 68Ga-PSMA 45- 60 min before the start of the image acquisition. 68Ga-PSMA PET/CT imaging of patients was performed using the General Electric Discovery PET/CT 600 device (GE Medical Systems, LLC, 3000 N. GRANDVIEW BLVD., WAUKESHA, WI., U.S.A.) First, CT imaging for attenuation correction and anatomical correlation was performed with a spiral 16-section scanner at 120 kV, 172 mAs, with an axial slice thickness of 2.5 mm. PET imaging was performed in 3-D, covering all parts of the body, including the cranium and feet, for about 3 minutes in each bed position. CT and PET images were matched and fused into transaxial, coronal, and sagittal images with an iterative reconstruction method. The data were transferred via the Digital Imaging and Communications in Medicine (DICOM) protocol to a processing Workstation (AW Volume Share5 GE Medical Systems S.C.S, France). Then, visual and semi-quantitative analyses were performed. The SUVmax computed by standard methods from the activity in the most intense voxel in the 3-D tumor region from the transaxial whole-body images. The maximum standardized uptake value (SUVmax) was calculated by the following formula: [Activity of ROI (mCi / ml) × Bodyweight (grams)] ÷ Injected dose (mCi)
Statistical Analysis
Statistical analyses were performed using the SPSS software version 22. The variables were investigated using visual (histograms, probability plots) and analytical methods (Kolmogrow-Smirnov/Shapiro-Wilk’s test) to determine whether or not they were normally distributed. The Chi-square test, or Fisher’s exact test where appropriate, was used to compare these proportions in different groups. While investigating the associations between non-normally distributed and/or ordinal variables, the correlation coefficients and their significance were calculated using the Spearman test. A p-value of less than 0.05 was considered to show a statistically significant result.
Results
All 75 patients included in the study, with a median age of 72 (range: 55-89), were adenocancer. Median HU 48.1 (range: 23.28-90.50), median SUVmax 11.5 (range:2-79) in the primary tumor area of the prostate gland, and median PSA value were measured as 32.85 g/mL (range: 4147 g/mL). Metastasis was present in 58 (77.3%) patients. Of the metastatic patients, 21 (28%) had lymph nodes and bone, 16 (21.3%) only bone, 9 (12%) only lymph nodes, 4 (5.3%) bone and lung, 3 ( 4%) lymph nodes, bone and lung, 2 (2.7%) bone and liver, 1 (1.3%) lung and lymph nodes, 1 (1.3%) brain, liver and bone, and 1 patient (1.3%) ) had bone, liver and lung metastases.
Systemic-immune-inflammation index (SII)
The median SII value was measured as 726.12 (range 50.62-5245.13), and no correlation was found between SII values and SUVmax, HU and PSA (p = 0.330, r = -0.114; p = 0.741, r = -0.039; p = 0.445, r = 0.092 respectively). When patients were divided into two groups according to their median SII values <726 and 726, a statistically significant difference was found between the groups in terms of lymph node metastasis (p = 0.007). Lymph node metastasis was found to be more common in patients with SII ≥ 726. However, there was no difference between the groups in terms of other metastasis patterns (distant organ metastasis, bone metastasis, and diffuse bone metastasis). Table 1 shows the relationship between metastasis patterns of prostate cancer and SII.
Neutrophil/lymphocyte ratio (NLR)
The median NLR value was 2.9 (range 0.72-26.63), so patients were examined in two groups as those with the NLR value <3 and ≥3. No correlation was found between NLR values and SUVmax, HU, and PSA (p=0.057, r=-0.221; p=0.253, r=-0.134; p=0.662, r=0.053, respectively). The relationship between metastasis pattern and NLR was found to be similar to SII values. While lymph node metastasis was statistically higher in patients with NLR value ≥3 (p=0.025), no difference was shown between the groups in terms of distant metastasis, bone metastasis, and widespread bone metastasis. Table 2 shows the relationship between prostate cancer metastasis patterns and NLR.
Platelet lymphocyte ratio (PLR)
The median PLR value was 153.57 (range 8.41-863.13), so patients were examined in two groups: PLR value <154 and ≥154. No correlation was found between PLR values and SUVmax, HU, and PSA (p=0.867, r=-0.020; p=0.607, r=-0.060; p=0.669, r=0.052, respectively). When patients were classified according to median PLR values, no statistically significant difference was found between the metastasis patterns of prostate cancer and the groups. Table 3 shows the relationship between prostate cancer metastasis patterns and PLR.
Mean platelet volume (MPV)
The median MPV value of the patients was 9.5 (range 7.10-11.20). No correlation was found between MPV values and SUVmax and HU (p=0.562, r=0.068; p=0.752, r=-0.037, respectively). However, a negative correlation was found between MPV values and PSA (p=0.008, r=-0.310). According to median MPV values, patients were divided into two groups: patients with MPV values <9.5 and ≥9.5, and diffuse bone metastasis was found to be higher in patients with MPV values < 9.5 (p=0.023). No differences were found between groups for other metastasis patterns.
Discussion
Prostate cancer incidence and morbidity have increased the most in recent years 11. Even if it is useful to reduce the level of androgens that are active in the development and progression of prostate cancer in the blood medically or surgically in the early stages of the disease, the disease becomes resistant to castration after a while. For this reason, it is important to determine prognostic factors before treatment. PSA is a tumor marker of both diagnostic and prognostic importance. Recently, many studies have been conducted on how peripheral inflammatory markers can predict cancer prognosis 12. Proinflammatory and immunosuppressive cytokines interfere with intracellular communication, regulate gene transcription, and play a role in promoting carcinogenesis in various tumor types, including prostate cancer 13. A complete blood test is an important test that provides more information about many diseases that are easily and cheaply used in the routine.
As with many other cancers, systemic inflammation in prostate cancers is known to play a role in both the development and progression of cancer 14. Systemic inflammation acts on neutrophils and cytokines, causing invasion and progression of tumor cells, while inhibition of lymphocytes, which provide regulation of the immune system, reduces the immune response to the tumor. For this reason, hematological biomarkers such as NLR and PLR are known to be prognostic factors in some cancers, and high levels are associated with poor prognosis 15,16. Recently, the systemic immune-inflammation index (SII) is also reported to be a similarly prognostic indicator for hepatocellular carcinoma, renal cell carcinoma, colorectal cancer, gastric cancer, and prostate cancer 17. The SII is a new inflammation index based on peripheral lymphocyte, neutrophil, and platelet counts. There is still a debate about the use of SII in urological cancers, but a growing number of studies have been conducted on this issue, and the sample size in the current research is not so large. According to the Man et al. study 17, high levels of SII and NLR in mCRPC patients were found to be associated with shorter overall survival. It is also known that progression-free survival after successive treatments with docetaxel and abiraterone is an important predictor of overall survival 18. In our study, no statistically significant association was found between all three inflammatory indices and survival analyses. However, it was thought that the biggest factor in this may be both the limitation of the number of patients and the short duration of follow-up.
Prostate-specific membrane antigen (PSMA) is a surface protein that is expressed at a low level in normal prostate tissue and at a much higher rate (about 1000 times) in prostate cancer tissue 19. 68Ga-PSMA PET/CT is an imaging method with high sensitivity and specificity for detecting recurrence despite low PSA levels in prostate cancer patients 20. It is a more accurate method for detecting lymph node metastases that are important in patient management, especially in moderate and high-risk patients 3. In castration-resistant disease, bones and lymph nodes are the most common areas of metastasis. The common lymph node metastasis sites for prostate cancer are the obturator, internal iliac, external iliac, common iliac, presacral, paraaortic and mediastinum, and supraclavicular lymph node. In our study, lymph nodes and bones were the most common metastatic areas, similar to the literature. It was found that lymph node metastasis was more frequent in patients with SII ≥ 726 than in those with low levels. It was also found that lymph node metastasis was more frequent in patients with NLR ≥ 3 than in those with lower levels. Contrary to the literature, no significant association was found between PLR and metastasis rates. In our study, we also found that diffuse bone metastasis was more common in patients with MPV < 9.5 in our patients.
According to the Cytawa et al. study 21, 68Ga-PSMA PET/CT is important for detecting nodal and/or distant metastases in the staging of moderate and high-risk prostate cancers, but it is not recommended for staging low-risk patients, as the prevalence of the extraprostatic disease is also low in low-risk patients. According to the same study, there is no significant relationship between PSA and SUVmax. In our study, there was no statistically significant relationship between PSA and SUVmax calculated from primary tumor localization in the prostate gland. However, in our study, there was a significant relationship between PSA levels and rates of metastasis in PET/CT. There was no significant relationship found between SII, NLR, PLR, and serum PSA levels, while a statistically significant relationship was observed between MPV and PSA. Because PSA is not a cancer-specific marker, it is a protein that can also be elevated in benign pathologies such as prostatitis and benign prostatic hyperplasia in patients who have not been diagnosed with cancer. However, if the patient has a diagnosis of prostate cancer, it becomes an important marker of disease recurrence. Mean platelet volume (MPV) is an indicator that shows platelet activity and platelet size. Low MPV levels are associated with inflammatory diseases and the reverse effect of anti-inflammatory therapy 22. It is also believed that it increases in prostate cancer, possibly due to the inflammatory effect caused by cancer.
Tables
Table 1. The relationship between SII and the metastasis pattern of prostate cancer

Median SII= 726.12 (range 50.62-5245.13)
Table 2. The relationship between NLR and the metastasis pattern of prostate cancer
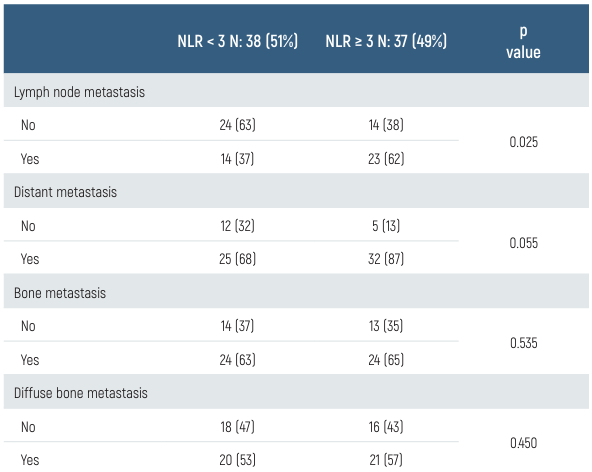
Median NLR= 2.9 (range 0.72-26.63)
Table 3. The relationship between PRL and the metastasis pattern of prostate cancer

Median PRL= 153.57 (range 8.41-863.13)
Limitations
The biggest limitation of our study was its retrospective design. For this reason, the infectious conditions of the patients could not be evaluated. Also, the small sample size was another important limitation.
Conclusion
As a result, a statistically significant relationship was found between high SII and high NLR values and lymph node metastasis. Also, a negative correlation between MPV and PSA, and a relationship between low MPV values and widespread bone metastasis were found. For this reason, it should be considered during clinical follow-up that both PSA levels, which are an important marker of metastasis in routine checks in patients with prostate cancer, and hemogram data, carry signs of possible metastasis. Also, it is believed that high levels of these inflammatory markers may reduce the effectiveness of cancer treatment and that anti-inflammatory treatments may also contribute to an additional contribution.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
-
Perera M, Papa N, Roberts M, Williams M, Udovicich C, Vela I, et al. Gallium-68 prostate- specific membrane antigen positron emission tomography in advanced prostate cancer: Updated diagnostic utility, sensitivity, specificity, and distribution of prostate-specific membrane antigen-avid lesions: A systematic review and meta-analysis. Eur Urol. 2020;77(4):403-17.
-
Peng L, Li J, Meng C, Li J, You C, Tang D, et al. Can 68Ga-prostate specific membrane antigen positron emission tomography/computerized tomography provide an accurate lymph node staging for patients with medium/high-risk prostate cancer? A diagnostic meta-analysis. Radiat Oncol. 2020;15(1):227.
-
Hegde PS, Chen DS. Top 10 challenges in cancer immunotherapy. Immunity. 2020;52(1):17-35.
-
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436-44.
-
Adhyatma KP, Prapiska FF, Siregar GP, Warli SM. Systemic inflammatory response in predicting prostate cancer: The diagnostic value of neutrophil-to-lymphocyte ratio. Open access Maced J Med Sci. 2019;7(10):1628-30.
-
Adhyatma KP, Warli SM. Diagnostic value of platelet-to-lymphocyte ratio in prostate cancer. Open access Maced J Med Sci. 2019;7(7):1093-96.
-
Tatenuma T, Kawahara T, Hayashi N, Hasumi H, Makiyama K, Nakaigawa N, et al. The pretherapeutic neutrophil-to-lymphocyte ratio for docetaxel-based chemotherapy is useful for predicting the prognosis of Japanese patients with castration-resistant prostate cancer. BioMed Res Int. 2019;2019:2535270.
-
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212-22.
-
Lolli C, Caffo O, Scarpi E, Aieta M, Conteduca V, Maines F, et al. Systemic immune- inflammation index predicts the clinical outcome in patients with mCRPC treated with abiraterone. Front Pharmacol. 2016;7:376.
-
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7-34.
-
Yamada Y, Sakamoto S, Rii J, Yamamoto S, Kamada S, Imamura Y, et al. Prognostic value of an inflammatory index for patients with metastatic castration-resistant prostate cancer. Prostate. 2020;80(7):559-69.
-
Hawley JE, Pan S, Figg WD, Lopez-Bujanda ZA, Strope JD, Aggen DH, et al. Association between immunosuppressive cytokines and PSA progression in biochemically recurrent prostate cancer treated with intermittent hormonal therapy. Prostate. 2020;80(4):336-44.
-
Langsenlehner T, Thurner EM, Krenn-Pilko S, Langsenlehner U, Stojakovic T, Gerger A, et al. Validation of the neutrophil-to-lymphocyte ratio as a prognostic factor in a cohort of European prostate cancer patients. World J Urol. 2015;33(11):1661-67.
-
Tatenuma T, Kawahara T, Hayashi N, Hasumi H, Makiyama K, Nakaigawa N, et al. The pretherapeutic neutrophil-to-lymphocyte ratio for docetaxel-based chemotherapy is useful for predicting the prognosis of Japanese patients with castration-resistant prostate cancer. BioMed Res Int. 2019;2019:2535270.
-
Donate-Moreno MJ, Lorenzo-Sánchez MV, Díaz de Mera-Sánchez Migallón I, Herraiz-Raya L, Esper-Rueda JA, Legido-Gómez O, et al. Inflammatory markers as prognostic factors in metastatic castration-resistant prostate cancer. Actas Urol Esp. 2020;44(10):692-700.
-
Man YN, Chen YF. Systemic immune-inflammation index, serum albumin, and fibrinogen impact prognosis in castration-resistant prostate cancer patients treated with first-line docetaxel. Int Urol Nephrol. 2019;51(12):2189-99.
-
Stangl-Kremser J, Mari A, Suarez-Ibarrola R, D’Andrea D, Korn SM, Pones M, et al. Development of a prognostic model for survival time prediction in castration-resistant prostate cancer patients. Urol Oncol. 2020;38(6):600.
-
Emmett L, Willowson K, Violet J, Shin J, Blanksby A, Lee J. Lutetium 177 PSMA radionuclide therapy for men with prostate cancer: a review of the current literature and discussion of practical aspects of therapy. J Med Radiat Sci. 2017;64(1):52-60.
-
Soydal C, Urun Y, Suer E, Nak D, Ozkan E, Kucuk NO. Predictor of 68Ga PSMA PET/CT positivity in patients with prostate cancer. Q J Nucl Med Mol Imaging. 2020;64(2):226-30.
-
Cytawa W, Seitz AK, Kircher S, Fukushima K, Tran-Gia J, Schirbel A, et al. 68Ga-PSMA I&T PET/CT for primary staging of prostate cancer. Eur J Nucl Med Mol Imaging. 2020;47(1):168-77.
-
Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011;17(1):47–58.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Seyit Ahmet Ertürk, Zekiye Hasbek, İsmail Şalk, Birsen Yücel, Özge Ulaş Babacan. Evaluation of the relationship between inflammatory markers (SII, NLR, PLR, and MPV) and diagnostic parameters of 68Ga-PSMA PET/CT in prostate cancer patients? Eu Clin Anal Med 2024;12(Suppl 1):S10-14
Publication History
- Received:
- August 26, 2024
- Accepted:
- October 17, 2024
- Published Online:
- October 19, 2024
- Printed:
- October 20, 2024
