Predisposition for atopy and pulmonary prognosis at preschool age of patients diagnosed with respiratory distress in the neonatal period
Effect of respiratory distress on atopy and lung prognosis
Authors
Abstract
Aim In this study, we aimed to determine the predisposition for atopy and pulmonary functions of patients who were followed up for respiratory distress syndrome in the neonatal period.
Material and Methods Fifty children hospitalized with respiratory distress in the neonatal period were included in the study, and the control group included 31 children, who had no respiratory problems, were included as the control group. Pulmonary function test was performed to evaluate the lung functions of the children included in the study. A Chest x-ray was performed. Total IgE and phadiaotope were studied in serum samples. A Skin prick test was done.
Results Serum total IgE results in the patient group were statistically significantly higher than in the control group (p=0.02). Of the 50 patients in the patient group, 5 (10%) had atopic asthma, 4 (8%) had nonatopic asthma, 2 (4%) had bronchopulmonary dysplasia, 2 (4%) had atopic dermatitis and 2 (4%) had allergic rhinitis. When 50 patients were examined in terms of atopy, 10 (20%) were considered atopic. In the control group, 1 child (3.2%) was considered atopic. Atopy was found to be statistically significantly higher in the patient group (p=0.03). Although the FVC, FEV1, FEV1/FVC and PEF values measured in the patient group were lower than those in the control group, the results were not statistically significant.
Discussion Diagnoses of atopic disease (atopic asthma, allergic rhinitis, atopic dermatitis), non-atopic asthma and bronchopulmonary dysplasia were found to be higher in patients followed up for respiratory distress in the neonatal period compared to the control group without respiratory problems.
Keywords
Introduction
Respiratory tract diseases are the most common cause of hospitalizations requiring special care in term and preterm infants [1]. Respiratory distress syndrome (RDS) is a disease that usually occurs in premature infants and develops due to surfactant deficiency. Its incidence increases with decreasing weeks of gestation and birth weight. Race, gender, maternal diseases, and antenatal glucocorticoid therapy affect the incidence [2, 3]. Allergic diseases have become an increasingly important health problem all over the world. The frequency of allergic diseases such as bronchial asthma, allergic rhinitis and atopic dermatitis is increasing both in our country and in many countries of the world [4, 5, 6]. It was determined that the lung functions of preterm- born children decreased significantly at school age [7, 8, 9, 10]. In addition, various studies investigating atopy in premature children have been conducted, some studies have shown that atopy is a reduced risk factor, while others have shown that there is no relationship between gestational age and atopy [10, 11, 12, 13, 14, 15, 16].
In this study, it was aimed to determine the respiratory functions and atopy susceptibility of preterm and term patients hospitalized for respiratory distress in the neonatal period and healthy children and to compare the results.
Materials and Methods
The study was conducted among the patients followed up with respiratory distress in the neonatal intensive care unit of Çukurova University Faculty of Medicine and healthy children born in the same period (2002-2005). Patients who accepted to participate in the study were invited to Çukurova University Faculty of Medicine Pediatric Allergy-Immunology outpatient clinic. Prenatal, birth, postpartum and family histories were questioned in detail. Systemic physical examination was performed in all children. All the information obtained was recorded in the questionnaire form. Eighty-one children aged 3-7 years were included in the study. Fifty children hospitalized with respiratory distress in the neonatal period were included as in the patient group. In the same period, 31 healthy children followed up for physiological jaundice were included in the study as a the control group. Pulmonary function test and chest x-ray were performed. Total IgE and phadiaotope were studied in serum samples. A skin prick test was done. Approval was obtained from families. The study was approved by the Ethics Committee of the Faculty of Medicine, Çukurova University (July 08, 2008, meeting number No. 8).
Statistical analysis
Statistical analysis of the study was performed using the Statistical Package for Social Sciences” version 17 (IBM Corp., Armonk, NY, USA) program. Whether the numerical measurements in the study group provided the assumption of normal distribution was tested with the Kolmogorovf- Smirnov test. Descriptive statistics of for parametric numerical data were calculated as mean ± standard deviation, non- parametric data were calculated as median (minimum-maximum, interquartile range), and categorical data were reportedgiven as percentage (%). The Chi-square test was used to compare categorical measurements between groups, the T- test was used for independent groups if the assumptions were met, and the Mann- Whitney U test was used if the assumptions were not met. A p-value < 0.05 was considered statistically significant.
Results
The mean age of 81 patients included in the study was 70±10.5 months. Fifty of the patients were in the group of those followed in the neonatal intensive care unit due to respiratory distress (patient group), and 31 were in the healthy control group. The gestational week of the children included in the study was between 28 and 39 weeks (Mean±SD: 35.01±2.92). Of the patient group, 16 (22.5%) had mild RDS, 19 (26.8%) had moderate RDS, and 15 (21.1%) had severe RDS. The mean age of the patient group was 67.2±11.2 months, and the mean age of the control group was 68.32±8.95 months. There was no significant difference between the groups in terms of age (p=0.63). Of In the patient group, 26 (52%) were male, 24 (48%) were female;, of in the control group, 14 (45.2%) were male and 17 (54.8%) were female. There was no significant difference between the groups in terms of gender (p=0.55). The mean body weight of the patient group was 20.38±3.49, and the mean body weight of the control group was 20.71±2.61 kg. There was no significant difference between the groups in terms of body weight (p=0.65).
The mean week of gestation of the patient group was 34±3.06 weeks, and the mean week of gestation of the control group was 36.65±1.74 weeks. There was a significant difference between the groups in terms of gestational week (p<0.001). Eight of the patient group were born by normal vaginal delivery (16%), 42 by cesarean section (84%), 9 of the control group were born by normal vaginal delivery (29%), and 22 by cesarean section (71%). There was no significant difference between the groups in terms of delivery type (p=0.16).
There was a family history of atopy in 22 (44%) of in the patient group and in 13 (41.9%) of in the control group (Figure 1). There was no statistically significant difference between the groups in terms of family history of atopy (p=0.85).
While serum total IgE results of the patient group were 99.6±119.46IU/ ml, it was 33.37±18.9 IU/ml in the control group (Table 1). When the groups were compared in terms of serum total IgE, a statistically significant difference was found (p=0.02). Since serum total IgE is affected by many factors, allergen-specific IgE values of all patients were also checked. Phadiaotope was positive in 6 (12%) of 50 patients in the patient group, and negative in all 31 patients in the control group. A statistically significant difference was found (p=0.04). When the food (Fx5) and mite (hx2) specific IgE results of the patient and control group cases were compared,; Fx5 was positive in 5 (10%) of 50 patients in the patient group, and Hx2 was found in 4 (8%) patients. All of the 31 patients in the control group had negative allergen-specific IgE results. Food allergy was detected in 10% of the patient group.
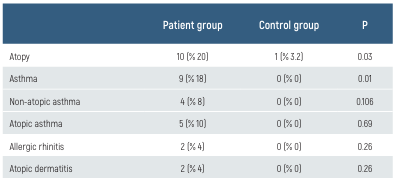
The skin test was positive in 8 (16%) of 50 patients in the patient group and in 1 (3.2%) of 31 patients in the control group (p=0.07). In the patient group, 5 of 50 patients (10%) had atopic asthma, 4 (8%) had nonatopic asthma, 2 (4%) had BPD, 2 (4%) had atopic dermatitis, 2 (4%) had allergic rhinitis. When the patient group was examined in terms of atopy, 10 (20%) were considered atopic. One child (3.2%) in the control group was considered atopic (Table 2). The difference between the groups in terms of total asthma number and atopy was statistically significant (p=0.03). Of the 50 patients in the patient group, 38 (76%) were premature and 12 (24%) were mature. Atopy was present in 7 (18.4%) of premature babies and 3 (25%) of mature babies. Of 31 patients in the control group, 15 (48.4%) were premature and 16 (51.6%) were mature. There was no atopy in premature babies, 1 (6.2%) of mature babies had atopy. When these data were evaluated statistically, there was no significant difference (p=0.092).
Discussion
In the cohort study conducted by Trønnes et al., asthma was 1.7 times more common in children with a history of preterm birth (32-36 weeks), 3.6 times more common in children with a history of extremely preterm birth (23-31 weeks) than in children born at term [17]. Preterm birth was associated with decreased odds of for severe atopic dermatitis (OR 0.9 (95% CI: 0.8–1.0) [17]. Although studies have evaluated atopy as an increased risk in premature babies, it is stated that environmental factors such as mechanical ventilation and family history of atopy may also affect the results. [18]. Pagano et al. stated that modifiable (gestational diabetes, antibiotic use) and non-modifiable (familiarity with asthma) conditions influence the risk of atopy in premature babies and showed that extreme prematurity reduced the risk of atopic dermatitis [19]. They also stated that premature babies showed a peculiar atopic march. [19]. In our study, no relationship was found between gestational week and atopy.
In the study conducted by Siltanen et al. in 72 premature patients and 65 mature control group children at the age of 10 years, atopic dermatitis was found in the preterm group at 22%, allergic rhinoconjunctivitis at 19%, atopic asthma at 5% and atopy at 30.6% in total. In the term group, 35.4% atopic dermatitis, 33.8% allergic rhinoconjunctivitis, 6.2% atopic asthma and 49.2% total atopy were detected [20]. In this study, it was shown that premature birth reduces the risk of atopy in the long term. In our study, when the patient group and control group were compared, a significant difference was found in terms of atopy (p=0.03). In the study performed by Siltanen et al., in 72 preterm and 65 term children at the age of 10, serum total IgE levels were found to be significantly higher in the mature group [20]. In the same study, serum allergen- specific IgE antibodies and skin test were found to be significantly higher in the mature group than in the premature group. The results of the study of by Trønnes et al. have shown that prematurity is associated with lower levels of IgE in serum and decreased occurrence of positive skin prick test reactions and allergic rhinitis [17]. In our study, serum Total IgE levels were found to be significantly higher in the patient group than in the control group. When the results of serum-specific IgE and skin tests were also compared, no significant difference was found between premature and mature patients in terms of atopy.
Figures
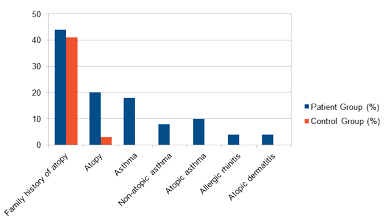
Figure 1. Atopy evaluation of the patient and control group.
Tables
Table 1. Comparison of allergy tests of patient and control groups.
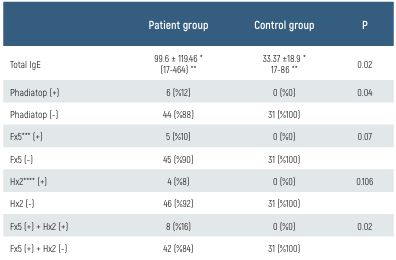
Table 2. Comparison of patient and control groups in terms of atopy.
Conclusion
In conclusion, 20% in the patient group and 3.2% in the control group were considered atopic. When the patient and control groups were compared in terms of atopy, there was a statistically significant difference (Table 2). While asthma (atopic+nonatopic) was present in 9 (18%) patients in the patient group, no asthma was detected in the control group. There was a significant difference when compared statistically. When compared in terms of pulmonary function test results, no significant difference was found, while chest x-ray radiography findings were found to be significantly compatible with chronic changes in the patient group. In addition, BPD was detected in 2 children in the patient group. However, there is a need for studies with larger patient and control groups on this subject, since the compliance of patients with pulmonary function test is insufficient and lung functions and atopy are affected by many genetic and environmental factors.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Baseer KAA, Mohamed M, Abd-Elmawgood EA. Risk Factors of Respiratory Diseases Among Neonates in Neonatal Intensive Care Unit of Qena University Hospital, Egypt. Ann Glob Health. 2020;86(1):22.
-
De Luca D, Tingay DG, van Kaam AH, Courtney SE, Kneyber MCJ, Tissieres P, et al. Neonatal ARDS Project Collaboration Group. Epidemiology of Neonatal Acute Respiratory Distress Syndrome: Prospective, Multicenter, International Cohort Study. Pediatr Crit Care Med. 2022;23(7):524-534.
-
De Luca D. Respiratory distress syndrome in preterm neonates in the era of precision medicine: A modern critical care-based approach. Pediatr Neonatol. 2021;62(Suppl.1):S3-9.
-
Gutowska-Ślesik J, Samoliński B, Krzych-Fałta E. The increase in allergic conditions based on a review of literature. Postepy Dermatol Alergol. 2023;40(1):1-7.
-
Gough H, Grabenhenrich L, Reich A, Eckers N, Nitsche O, Schramm D, et al. MAS study group. Allergic multimorbidity of asthma, rhinitis and eczema over 20 years in the German birth cohort MAS. Pediatr Allergy Immunol. 2015;26(5):431-7.
-
Sigurdardottir ST, Jonasson K, Clausen M, Lilja Bjornsdottir K, Sigurdardottir SE, Roberts G, Grimshaw K, et al. Prevalence and early-life risk factors of school-age allergic multimorbidity: The EuroPrevall-iFAAM birth cohort. Allergy. 2021;76(9):2855-2865.
-
Thunqvist P, Tufvesson E, Bjermer L, Winberg A, Fellman V, Domellöf M, et al. Lung function after extremely preterm birth-A population-based cohort study (EXPRESS). Pediatr Pulmonol. 2018;53(1):64-72.
-
Chang HY, Chang JH, Chi H, Hsu CH, Lin CY, Jim WT, et al. Reduced Lung Function at Preschool Age in Survivors of Very Low Birth Weight Preterm Infants. Front Pediatr. 2020 22;8:577673.
-
Er İ, Günlemez A, Uyan ZS, Aydoğan M, Oruç M, Işık O, et al. Evaluation of pulmonary functions in preschool children born late-preterm. Turk Arch Pediatr. 2017;52(2):72-78.
-
Guimarães H, Rocha G, Pissarra S, Guedes MB, Nunes T, Vitor B. Respiratory outcomes and atopy in school-age children who were preterm at birth, with and without bronchopulmonary dysplasia. Clinics (Sao Paulo). 2011;66(3):425-30.
-
Pagano F, Conti MG, Boscarino G, Pannucci C, Dito L, Regoli D, et al. Atopic Manifestations in Children Born Preterm: A Long-Term Observational Study. Children (Basel). 2021;8(10):843.
-
Siltanen M, Wehkalampi K, Hovi P, Eriksson JG, Strang-Karlsson S, Järvenpää AL, et al. Preterm birth reduces the incidence of atopy in adulthood. J Allergy Clin Immunol. 2011;127(4):935-42.
-
El-Heis S, Crozier SR, Healy E, Robinson SM, Harvey NC, Cooper C, et al. Southampton Women’s Survey Study Group. Faltering of prenatal growth precedes the development of atopic eczema in infancy: cohort study. Clin Epidemiol. 2018;10:1851-1864.
-
Kowalik A, Cichocka-Jarosz E, Kwinta P. Atopic dermatitis and gestational age - is there an association between them? A review of the literature and an analysis of pathology. Postepy Dermatol Alergol. 2023;40(3):341-349.
-
Barbarot S, Gras-Leguen C, Colas H, Garrot E, Darmaun D, Larroque B, et al.. Lower risk of atopic dermatitis among infants born extremely preterm compared with higher gestational age. Br J Dermatol. 2013;169(6): 1257-64.
-
Egeberg A, Andersen YM, Gislason G, Skov L, Thyssen JP. Neonatal risk factors of atopic dermatitis in Denmark - Results from a nationwide register-based study. Pediatr Allergy Immunol. 2016;27(4):368-74.
-
Trønnes H, Wilcox AJ, Lie RT, Markestad T, Moster D. The association of preterm birth with severe asthma and atopic dermatitis: a national cohort study. Pediatr Allergy Immunol. 2013;24(8):782-7.
-
Liem JJ, Kozyrskyj AL, Huq SI, Becker AB. The risk of developing food allergy in premature or low-birth-weight children. J Allergy Clin Immunol. 2007;119(5):1203-9.
-
Pagano F, Conti MG, Boscarino G, Pannucci C, Dito L, Regoli D, et al. Atopic Manifestations in Children Born Preterm: A Long-Term Observational Study. Children (Basel). 2021;8(10):843.
-
Siltanen M, Kajosaari M, Pohjavuori M, Savilahti E. Prematurity at birth reduces the long- term risk of atopy. J Allergy Clin Immunol. 2001;107(2):229-34.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
None of the authors received any type of financial support that could be considered potential conflict of interest regarding the manuscript or its submission.
Ethics Declarations
This study was approved by the Ethics Committee of Faculty of Medicine, Çukurova University (Date: 2008-08-07, No: 8)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Asena Ünal, Seval Güneşer Kendirli. Predisposition for atopy and pulmonary prognosis at preschool age of patients diagnosed with respiratory distress in the neonatal period. Eu Clin Anal Med 2024;12(1):1-4
Publication History
- Received:
- September 7, 2023
- Accepted:
- October 21, 2023
- Published Online:
- November 30, 2023
- Printed:
- January 1, 2024
