Innovative approaches to neutralizing sympathetic nerves in addressing focal hyperhidrosis
Innovative approaches to focal hyperhidrosis
Authors
Abstract
The article addresses the complexity of Focal Hyperhidrosis (localized excessive sweating) and discusses its impact on individuals’ social, professional, and psychological lives. This condition, which affects 1-3% of the U.S. population, is most commonly seen in areas like hands, feet, underarms, and face. Primary hyperhidrosis is more prevalent and is associated with genetic factors. Determining a diagnosis for hyperhidrosis relies on observing the symptoms during a clinical examination and understanding the patient’s medical background. The condition can greatly disrupt a person’s daily life due to excessive sweating. There are various treatment options available, including topical antiperspirants, Botox injections, iontophoresis, or anticholinergic medications. There are also more invasive procedures like microwave therapy, laser therapy, Endoscopic Thoracic Sympathectomy (ETS), or liposuction. The article highlights the importance of effectively managing hyperhidrosis and acknowledges the psychological and social challenges associated with it.
Keywords
Introduction
Sweating, a natural mechanism, aids in preserving our body’s thermal balance. Nonetheless, certain individuals experience this mechanism overly, exhibiting more sweating than typical. For some, it pervades the entirety of their body, while others might observe it in specific regions. In this article, we will explore the phenomenon of localized excessive sweating, known as Focal Hyperhidrosis. This particular condition is characterized by the regular occurrence of excessive sweating in specific areas of the body, including the hands, feet, underarms, and face. The manifestation of localized profuse sweating in these regions can give rise to a range of challenges that impact individuals in their social interactions, professional pursuits, and psychological life.
With the advancement of technology, touchscreen phones and tablets have become integral parts of our daily lives. However, for individuals who experience excessive sweating in their hands, these devices pose an additional challenge. Sweaty hands not only make it difficult to use touchscreens effectively but also exacerbate discomfort, especially when dealing with this issue in social settings or crowded environments. In densely populated areas, the problem of sweaty hands can be particularly pronounced, affecting individuals to a greater extent 3. This article scrutinizes literature that elaborates on the causes, effects, and methods of treating localized excessive sweating. The intention is to highlight the issue of excessive sweating that negatively impinges on the quality of life of individuals and to survey the solution pathways and existing literature information on the topic.
Epidemiology
Hyperhidrosis is a condition of excessive sweating that affects 1-3% of the population in the United States 4. However, less than half of those affected seek medical attention. The most common type, primary hyperhidrosis, is observed in the axillary region in half of the cases. One-third of patients with axillary hyperhidrosis believe that this issue is detrimental to their lives. Two-thirds of patients report a family history, which suggests a potential genetic link. Women tend to consult doctors more frequently than men 4.
The sympathetic nervous system regulates the body’s ability to maintain thermal balance through sweating. The primary types of sweat glands are eccrine and apocrine. Apocrine glands produce a distinct odor as a result of bacterial decomposition. Sweating increases with temperature, activity, or stress.
Hyperhidrosis denotes excessive sweating, particularly in specific areas such as the underarms. Night sweats are typically not present. This condition affects 2-4% of the population and its specific cause is unknown. The prevalence of hyperhidrosis can vary depending on the geographic region. For instance, it has been found to be 2.8% in the USA 5,3. There is literature support for the possibility of a genetic transmission of hyperhidrosis, and it is particularly thought to be possibly associated with the 14th chromosome 6.
Pathophysiology
Sweating is a mechanism that maintains the body’s thermal equilibrium. However, excessive sweating, medically termed hyperhidrosis, is observed in certain regions of some individuals. This study aims to examine the mechanisms of formation and the regions affected by hyperhidrosis.
The human body contains approximately 4 million sweat glands. A substantial majority of these, around 3 million, are eccrine sweat glands. Eccrine sweat glands produce sweat, a colorless and odorless liquid that regulates body temperature. These glands are especially concentrated in the palms, soles, craniofacial area, and axillary regions. On the other hand, the remaining sweat glands are of the apocrine type and are particularly located in the axillary and urogenital regions. Apocrine sweat glands do not play a direct role in the phenomenon of excessive sweating 3,7.
Although the precise etiology of hyperhidrosis remains uncertain, it is hypothesized to originate from heightened stimulation of the sympathetic nervous system by the hypothalamus, leading to overactive eccrine sweat glands. Hyperhidrosis can be influenced by genetic factors, hormonal imbalances, and certain medical conditions. This excessive sweating condition commonly manifests in localized regions, including the hands, feet, underarms, and face. Notably, facial sweating is known to occur in response to emotional stimuli or postprandial reactions 3.
The sweating mechanism is controlled by the hypothalamus’s thermoregulatory center. A chemical mediator named acetylcholine plays a significant role in this control mechanism. Activating stimuli activate the hypothalamus, leading to the release of acetylcholine. In individuals experiencing excessive sweating, there is a potential disruption in the equilibrium of these physiological pathways, impeding the body’s ability to maintain homeostasis 3,7.
Hyperhidrosis is characterized by the occurrence of excessive sweating in specific regions of the body. This excessive activation of eccrine sweat glands is a result of heightened stimulation of the hypothalamus. A comprehensive understanding of the underlying pathophysiological mechanisms is crucial for the development of effective treatment approaches. By gaining insights into these causes, more targeted and successful treatment methods can be devised.
Diagnosis
The diagnosis of hyperhidrosis primarily hinges upon clinical findings, taking the patient’s medical history and physical examination as a foundational basis. In the case of primary hyperhidrosis, sweating is frequently observed in areas such as the hands, armpits, feet, and face. The accurate categorization and diagnosis of this type of hyperhidrosis are facilitated by considering specific criteria 8.
Instead of a list, the diagnostic criteria for primary sweating disorder are concisely summarized in the table below: (References: 9,10).
The sweating mechanism is utilized to regulate body temperature. In some physiological conditions, the sweat glands can be observed to be overly active. Excessive sweating can be classified into two primary categories: primary (focal) hyperhidrosis and secondary (compensatory) hyperhidrosis. It is essential to differentiate between these two types. Secondary hyperhidrosis is often linked to underlying medical conditions such as infections, tumors, or hormonal imbalances. In contrast, primary hyperhidrosis is observed in otherwise healthy individuals and is not attributed to an underlying disease 4.
There are currently no definitive controlled studies available for the diagnosis or severity assessment of primary hyperhidrosis. Among the diagnostic criteria, sweating must continue for more than six months and must be distinctly focal. Also, in patients who meet the diagnostic criteria, there must be at least two characteristics such as bilateral and symmetric sweating, impairment of daily activities, at least one episode per week, onset before the age of 25, absence of sweating during sleep, and a positive family history 9,10. These four characteristics make the distinction between primary and secondary hyperhidrosis clearer. Laboratory tests are generally unnecessary in situations where an underlying cause is not suspected. The potential underlying causes of hyperhidrosis vary significantly.
Hyperhidrosis can have significant negative impacts on various aspects of daily life, including emotional well-being, self-esteem, social relationships, and work productivity. To assess the impact of sweating on quality of life, several measurement tools have been developed. One such tool is the Hyperhidrosis Disease Severity Scale (HDSS), which employs a four-level questionnaire system to gauge the tolerability of sweating and its consequences on daily activities. This survey serves as a predictive tool for evaluating the effects of hyperhidrosis on daily functioning and response to treatment. The HDSS scoring is as follows: 1 point indicates unnoticed sweating without affecting daily activities, 2 points correspond to tolerable sweating that occasionally affects daily activities, 3 points represent difficult-to-tolerate sweating that frequently affects daily activities, and 4 points reflect intolerable sweating that consistently disrupts daily activities. Scores of 1 or 2 are categorized as mild, while scores of 3 or 4 indicate severe hyperhidrosis 9,11,12.
Complaints
Excessive sweating, specifically primary hyperhidrosis, occurring in the hands, feet, underarms, and facial regions, gives rise to a constant feeling of dampness and humidity. Patients often find this condition bothersome, as the moisture resulting from excessive sweating creates an environment conducive to the growth of bacteria. Consequently, unpleasant odors may develop, leading to self-consciousness. Additionally, the excessive sweating can cause stains on clothing, which can be visually unappealing to the individual.
Therefore, the patient might be constrained in their clothing choices. It can adversely affect social interactions and professional relationships. The patient might tend to avoid normal social interactions, such as handshaking. It can diminish the individual’s self-esteem and confidence. Consequently, the patient may experience psychological stress. It can negatively impact daily activities and work productivity. Especially those experiencing sweating issues at the workplace might be unable to perform their jobs with full efficiency. The patient may describe personal discomfort and a continuous sensation of wetness caused by excessive sweating. These complaints are common discomforts experienced by the patient due to primary hyperhidrosis 12.
Treatment
Excessive sweating (primary hyperhidrosis) in the hands, feet, underarms, and face areas can be treated with medical and surgical methods. The following are some treatment options used in these regions:
Antiperspirants
Potent antiperspirants designed for application on the hands, feet, and underarm regions play a crucial role in offering temporary relief from excessive sweating. These topical products are formulated to diminish the activity of sweat glands by employing aluminum salts as their active ingredient. By obstructing the sweat gland ducts, antiperspirants effectively mitigate perspiration, which can provide a practical solution for managing hyperhidrosis. 4,13.
The usage of antiperspirants is quite simple:
Before applying antiperspirant, clean the areas that produce sweat (e.g., underarms) and thoroughly dry them. Clean skin enhances the efficacy of the product. Antiperspirants are usually applied before going to bed at night. This is when sweat glands are least active, and it aids the product to be more effective. There is no need to use the product excessively. Applying a thin layer is sufficient. After applying the antiperspirant, leave the area to dry. It will dry gradually and begin to reduce sweating. In the morning when you wake up, you may wish to reapply the antiperspirant to the same area, but the effect of the product applied overnight will still be ongoing 4,13.
Antiperspirants are over-the-counter products and are available in various brands and formulations. Each antiperspirant has different strengths, so it is important to follow the recommended dosage carefully.
Botox
Botox is a toxin produced by the Clostridium botulinum bacterium, and it may reduce sweating by temporarily reducing the excessive activity of sweat glands. Botox is injected into the ends of the sweat glands where it blocks nerve stimulation of the glands.
Botulinum toxin (Botox) injections can assist in controlling excessive sweating, and they are particularly effective in the underarm area. This treatment provides a temporary blockade of sweat glands, and the results generally works between 4-6 months 11.
Before deciding on Botox treatment, the severity of the excessive sweating issue and the affected areas are evaluated. Using Botox is typically considered when the excessive sweating issue is taken seriously or when other treatment options have failed. The patient’s medical history and the effects of sweating on their life are also taken into account.
Before applying Botox as a treatment, the patient is examined by a doctor to evaluate the sweating issue. The areas that need to be treated are identified. Prior to Botox application, the area is cleaned, and local anesthesia may be applied for the comfort of the patient. Botox is injected into specific areas of the sweat glands using a fine needle. Depending on the severity of the sweating issue, a varying number of injections may be performed. The results of Botox treatment usually begin to be noticed within a few days. Sweating reduces due to the temporary blockade of sweat glands. The results usually last between 4 to 6 months.
Dosage can vary depending on the area treated and the patient’s needs. The Botox dose applied to a particular area generally varies between 50 and 100 units 11. However, these dosages are adjusted according to the patient’s specific needs and determined by a doctor. Although Botox treatment is generally safe, some potential complications might include:
• Pain, swelling, or bruising at the injection site.
• Temporary numbness or tingling in the areas where injections were administered.
• Rarely, side effects that can lead to general muscle weakness.
These complications are typically temporary and can be managed by a healthcare professional 11.
Lontophoresis
This treatment method is particularly effective for hands and feet. Iontophoresis devices allow a low current in the water to temporarily close the sweat glands on the skin surface. Several sessions per week may be required. Iontophoresis is a treatment option utilized to control excessive sweating 4,10.
Iontophoresis devices facilitate the easy application of this treatment method.
Before deciding on iontophoresis treatment, the severity and the areas affected by excessive sweating are assessed. This treatment is usually effective in cases where excessive sweating ranges from mild to moderate 4,10.
Iontophoresis treatment involves the following steps: Prior to treatment, the excessively sweating areas are cleaned. Once the areas are dried, the iontophoresis device is used. The iontophoresis device applies a low current through the water to the skin surface. There are typically specialized devices available for hands and feet. The settings on the device help personalize the treatment. An iontophoresis session generally lasts between 20 and 40 minutes. Depending on the severity of sweating, several sessions per week may be required. The results of iontophoresis treatment typically begin to be noticed after a few sessions. Sweating reduces due to the temporary blockade of sweat glands. The results can often be long-lasting 4,10.
Although iontophoresis treatment is generally safe, some potential complications may arise. These complications may include incorrect use of the iontophoresis device or overly frequent application of therapy can lead to skin irritation. Those with sensitive skin are at risk. Mild pain or discomfort may be experienced during iontophoresis. This may be part of the process of getting used to the treatment. Temporary electrolyte imbalance may occur due to the absorption of water by the skin during iontophoresis. Therefore, it is important to drink enough water during treatment. Iontophoresis may not be effective for everyone 4,10.
Anticholinergic Medications
Anticholinergic medications function by blocking the impact of acetylcholine, a neurotransmitter involved in the nervous system. They are utilized to regulate the overactive function of sweat glands and can effectively alleviate hyperhidrosis, the condition of excessive sweating. In managing hyperhidrosis, healthcare professionals may suggest the use of anticholinergic drugs. However, these medications can frequently lead to side effects and should be managed with caution 4. Before making a decision regarding the use of anticholinergic medications, the severity of sweating and the specific areas affected are taken into consideration. This treatment option is typically considered when other approaches have proven ineffective or when excessive sweating is significantly impacting the individual’s quality of life.
A suitable anticholinergic drug is selected depending on the patient’s condition and the intensity of the sweating. Dosage is determined based on the specific needs and side effects experienced by the patient. The medication dosage may be low at the start of treatment and can be increased over time. Anticholinergic drugs are usually taken orally. The patient is guided regarding usage instructions and dosage. The patient should maintain regular communication throughout the treatment process. Adjustments in dosage or management of side effects may be required 4.
Although anticholinergic medications are generally safe, some potential complications may arise. These complications might include: One side effect of anticholinergic medications is dry mouth, which can be alleviated by measures like drinking plenty of water or using sugar-free gum. Headache, another side effect, should be reported to a healthcare professional if it is severe or persistent. Some anticholinergic drugs can cause temporary vision problems; anyone experiencing vision issues should immediately contact a healthcare professional. Other side effects associated with the use of the medications may include constipation, urinary retention, and indigestion 4.
Microwave Therapy
Microwave therapy is a non-invasive treatment approach used for the management of hyperhidrosis. By harnessing microwave energy, this innovative method specifically focuses on the sweat glands. The application of microwave energy to the sweat glands temporarily disrupts their functionality, resulting in a reduction of sweating. This treatment option offers the potential for long-lasting results, although multiple sessions may be necessary in some cases to achieve the desired outcome 4.
Before deciding to utilize microwave therapy, the severity of the sweating and the affected regions are evaluated. This treatment is typically considered when other methods have failed or the issue of excessive sweating is taken seriously by the patient.
Before the treatment begins, areas that sweat excessively are cleaned. After drying the areas, the microwave therapy device is used. The device applies microwave energy to areas where excessive sweating is concentrated. The settings of the device aid in personalizing the treatment. The duration and intensity of the microwave therapy session may vary, depending on the severity and need of the treatment. Results are usually noticed after several sessions 4.
Microwave therapy devices can be manufactured by different brands, and the name of the device might change according to the manufacturer. These devices should be used by specialists and adjusted according to patient needs. The frequency and duration of application can often vary based on the effectiveness of the treatment and the patient’s response.
Although microwave therapy is usually considered a safe treatment option, some potential complications can arise. These complications might include skin irritation, which can occur in the areas where the treatment is applied. This can be prevented by preparing the treatment area and performing skin care. Mild pain or discomfort might be felt during microwave therapy. This is generally temporary and provides relief post-treatment. Rarely, side effects such as headache or dizziness may occur due to microwave therapy 4.
Laser
Laser therapy can be utilized to treat excessive sweating, particularly in the facial area. The laser can aid in damaging the sweat glands, however, its effects may vary between individuals and multiple sessions may be required.
Laser therapy involves applying high-energy laser beams to the sweat glands. This helps to treat hyperhidrosis by affecting the glands, which leads to reducing excessive perspiration.
Before deciding to use laser therapy, the severity and affected areas of excessive sweating are evaluated. This treatment is typically considered when other methods have been ineffective or when the issue of hyperhidrosis is taken seriously.
Before the treatment begins, areas of excessive sweating are cleansed and the skin surface is coated with a special gel. This gel facilitates better penetration of the laser beams into the skin. The laser therapy device administers high-energy laser beams to the sweat glands. The skin surface is not harmed during this procedure as the laser beams target only the sweat glands. Laser therapy sessions typically last between a few minutes to an hour, varying based on the size and severity of the treatment areas 5.
Laser therapy devices can be produced by various brands and models, and the name of the device might differ according to the manufacturer. The frequency and duration of application are adjusted based on the efficacy of the treatment and the patient’s needs. Generally, results begin to be noticeable after a few sessions 5.
Although laser therapy is generally considered a safe treatment option, some potential complications might arise. These complications can include skin irritation or burns during the laser therapy procedure, hence undergoing the treatment under the supervision of an experienced healthcare professional is vital. Temporary pigment changes in the skin may occur post-laser therapy, which typically resolve over time. There’s a risk of infection after the treatment, so proper wound care and adherence to hygiene rules are essential. Mild pain or discomfort may be experienced during the treatment, which is usually alleviated post-procedure 5.
Surgical Options
When non-surgical treatment methods are insufficient, surgical options might be considered. The choice of treatment should be determined based on the degree of the patient’s sweating, the areas affected, and personal preferences.
Endoscopic Thoracic Sympathectomy (ETS)
Endoscopic Thoracic Sympathectomy (ETS) is an effective surgical treatment, particularly for excessive sweating in the hands, face, and underarms. It’s also used in treating conditions like facial blushing and Raynaud’s phenomenon. This procedure inhibits the overactivity of sweat glands by cutting or blocking the sympathetic nerves (Figure 1). It is executed with a minimally invasive approach, hence recovery time is short and effects are quickly apparent 5.
During the operation, while the patient is under general anesthesia, an endoscopic camera and surgical instruments are inserted into the chest wall through millimetric incisions. The sympathetic nerves visualized with the camera are clamped at the determined level o stop their influence on sweating. Post-procedure, the incisions are closed with sutures or surgical tape 5.
However, ETS has potential side effects. The most common side effect is compensatory sweating, where decreased sweating in the treated area results in increased sweating in other parts of the body, especially the back and legs. Horner’s Syndrome is a rarer side effect. It causes symptoms like drooping eyelids and miosis in one eye. Additionally, temporary pains in the chest or back may occur post-operation. Like any surgical procedure, ETS carries risks of infection, bleeding, and anesthesia 5.
ETS can permanently solve the problem of excessive sweating. However, it comes with its own advantages as well as disadvantages and risks.
Liposuction
Hyperhidrosis, commonly known as excessive sweating, can cause not only physical but also social and emotional distress for individuals. There are various treatment methods to address complaints of excessive sweating, one of which is liposuction.
Liposuction, typically utilized for fat removal, is also an effective method for removing sweat glands in hyperhidrosis treatment. This procedure, targeting excessive sweating in the armpit area in particular, aims to reduce sweating by directly extracting sweat glands.
After numbing the armpit area with local anesthesia, the surgeon uses a thin tube (cannula) to suction the sweat glands. After the sweat glands are removed via the cannula, the procedure is concluded. Entry points are closed with stitches or special tapes. The operation usually takes less than an hour 4.
This minimally invasive procedure, which does not require stitches and usually offers a rapid recovery time, has the potential to provide long- term permanent results by directly removing sweat glands. However, removing all sweat glands is not always guaranteed. Liposuction may be more costly compared to other treatment methods and also carries risks of infection, bleeding, bruising, and minor scarring 4.
Liposuction can be a treatment alternative for individuals with complaints of excessive sweating.
Curettage
Curettage is a preferred method in the surgical treatment of excessive sweating. This procedure, applied especially for patients who do not respond to medical treatments, aims to remove sweat glands causing excessive sweating in the armpit area.
After numbing the armpit with local anesthesia, the sweat glands are scraped and removed with a tool called a curette. After the procedure, the treated area is closed either with stitches or special tapes 14.
The advantage of this method is that it can usually provide permanent and effective results in a single session by directly removing the sweat glands. However, it carries typical surgical risks such as minor scarring, infection, bleeding, or bruising after curettage. As removing all sweat glands is not always guaranteed, it is not certain whether sweating will completely cease. The recovery time may be longer compared to some other treatments.
Curettage is a surgical approach with the potential to permanently solve the excessive sweating issue 14.
Other Methods:
Micro ETS
A more specific version of Endoscopic Thoracic Sympathectomy, implemented as a surgical procedure with smaller incisions 15.
Closed Sympathectomy
Used to treat axillary hyperhidrosis, it involves disabling the sympathetic nerves with an intravenous catheter or radiofrequency energy.
Micro-Phrenic Sympathectomy
Another method used to treat excessive sweating in the chest area involves the cutting of sympathetic nerves.
There may be specific methods for excessive sweating in other areas, such as the face and feet. However, these methods are generally rarely applied and lack distinct standards. The differences between these surgical methods depend on factors like which area they are used to treat, the complexity of surgical techniques, and side effects. The choice of method is determined based on the patient’s specific condition, the severity of symptoms, and the patient’s consent to surgery.
Figures
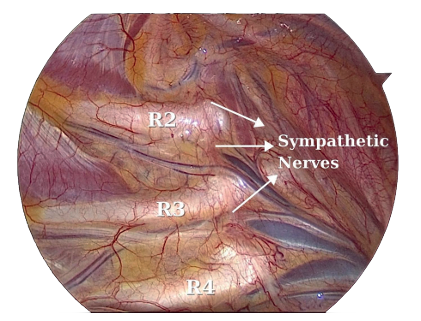
Figure 1. Thoracic Sympathetic Nerves (Endoscopic Thoracic Sympathectomy)
Tables
Table 1. Diagnostic Criteria for Primary Sweating Disorder

Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Ho YL, Jamaluddin MF, Krishinan S, Abdul Kareem BA. Diagnosis, impact and management of hyperhidrosis including endoscopic thoracic sympathectomy. Med J Malaysia. 2020;75(5):555-560.
-
Hirakawa N, Higashimoto I, Takamori A, Tsukamoto E, Uemura Y. The impact of endoscopic thoracic sympathectomy on sudomotor function in patients with palmar hyperhidrosis. Clin Auton Res. 2021;31(2):225-230.
-
Wolosker N, Campos JRM, Kauffman P, Silva MFA, Faustino CB, Tedde ML et al. Twenty years of experience with bilateral video assisted thoracic sympathectomy (VATS) for hyperhidrosis treatment in 2431 patients: A Cohort Study. Sao Paulo Med J. 2022;140(2):284-9.
-
McConaghy JR, Fosselman D. Hyperhidrosis: Management Options. Am Fam Physician. 2018;97(11):729-734.
-
Xie H, Lu T, Zhu Y, Zhu D, Wei T, Yuan G et al. A retrospective cohort study of T3 versus T4 thoracoscopic sympathectomy for primary palmar hyperhidrosis and primary palmar hyperhidrosis with axillary and plantar sweating. Videosurgery Miniinv. 2020;15(3):488–495.
-
Zhang D, Zhuang W, Lan Z, Huang S, Gao Z, Chen Q et al. Long-term follow-up in quality of life before and after endoscopic thoracic sympathicotomy in 367 patients with palmar hyperhidrosis. Ann Palliat Med. 2022;11(6):1961-1968.
-
Önder M, Aksoy G. Hyperhidrosis. Türkderm. 2011;45:2-9.
-
Kuijpers M, Peeters G, Harms PW, Bouma W, DeJongste MJ, Mariani MA et al. Bilateral one-stage single-port sympathicotomy in primary focal hyperhidrosis, a prospective cohort study: treat earlier? J Cardiothorac Surg. 2021;16(1):50.
-
Özcan D, Güleç AT. Hiperhidroz ve Tedavisi: Palmoplantar Hiperhidroz. Tedavisinde Güvenli ve Etkili Bir Seçenek, Ðyontoforez. Turk J Dermatol. 2011;5:5-12.
-
Alhetheli G. Outcome using either intradermal Botox injection or endoscopic thoracic Sympathectomy for patients with primary palmar hyperhidrosis: A Comparative Study. Cosmetics. 2021;8(2):41.
-
Moon MH, Hyun K, Park JK, Lee J. Surgical treatment of compensatory hyperhidrosis: Retrospective observational study. Medicine. 2020;99(42):e22466.
-
Kuijpers M, van Zanden JE, Harms PW, Mungroop HE, Mariani MA, Klinkenberg TJ et al. Minimally invasive Sympathicotomy for palmar hyperhidrosis and facial blushing: current status and the hyperhidrosis expert center approach. J Clin Med. 2022;11(3):786.
-
Felisberto G Jr, Cataneo AJM, Cataneo DC. Thoracic sympathectomy for the treatment of primary axillary hyperhidrosis: systematic review and proportional meta-analysis. Ann Med. 2021;53(1):1217-1227.
-
Raveglia F, Orlandi R, Guttadauro A, Cioffi U, Cardillo G, Cioffi G et al. How to prevent, reduce, and treat severe post sympathetic chain compensatory hyperhidrosis: 2021 State of the Art. Front Surg. 2022;8:814916.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None
Conflict of Interest
The authors declare no conflicts of interest.
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Orhan Yucel, Fatma Elcim, Zarife Jale Yucel. Innovative approaches to neutralizing sympathetic nerves in addressing focal hyperhidrosis. Eu Clin Anal Med 2024;12(1):12- 17
Publication History
- Received:
- December 2, 2023
- Accepted:
- December 30, 2023
- Published Online:
- January 1, 2024
- Printed:
- January 1, 2024
