The relationship of CURB65-L and CURB65-LC (lactate clearance) with mortality in pneumonia patients admitted to the emergency department
CURB65, lactate and pneumonia
Authors
Abstract
Aim The study aims to examine the correlation between lactate, lactate clearance, CURB-65, CURB65-L, and CURB65-LC scores with mortality in pneumonia patients who were admitted to the emergency department.
Material and Methods A total of 123 patients diagnosed with pneumonia who applied to the emergency department were assessed prospectively. Lactate clearance (%): [lactate at admission – lactate at 24th hour / lactate at admission) × 100]. Statistical comparisons were made across patient groups based on lactate, lactate clearance, and CURB-65 scores. These groups included survivors and non-survivors, patients in the intensive care unit and those who were not, patients receiving mechanical ventilation and vasopressor support, and those who did not, as well as patients with a hospital stay ≤10 days and those with a hospital stay > 10 days.
Results Among patients with severe illness who did not survive and required intensive care unit admission, mechanical ventilation and vasopressor support, the lactate and CURB-65 scores were significantly higher, while the lactate clearance score was lower (p < 0.001 for all). The predictive power of CURB65-L and CURB65-LC for mortality was determined to be higher than CURB-65 and lactate clearance alone (AUC: 0.904, 0.855, 0.783, 0.834, respectively) (p<0.001 for all).
Discussion The presence of lactate, the CURB-65 score, and lactate clearance level assessed upon admission to the emergency department can serve as predictors of negative results in patients with pneumonia. In addition, the combination of CURB65-L and CURB65-LC enhances the predictive power of CURB-65 and LC individually in determining mortality.
Keywords
Introduction
Community Acquired Pneumonia (CAP), classified as a medical emergency, is one of the leading causes of acute respiratory failure, sepsis, shock, and mortality. Furthermore, pneumonia has been found as the primary factor leading to unanticipated admission to the intensive care unit (ICU) within the initial 24 hours following presentation at the emergency department (ED) [1]. To enhance outcomes in these patients, it is crucial to make prompt and efficient decisions regarding triage, discharge, or hospitalization [2].
Lactate, produced by the reduction of pyruvate by the lactate dehydrogenase enzyme, is a marker that can be easily detected in venous blood gas (VBG). Its concentration in the blood rises in response to situations such as tissue hypoxia and hypoperfusion [3]. Elevated lactate levels during hospitalization are associated with increased mortality, the need for mechanical ventilation (MV), a requirement for vasopressors support (VS), and a high incidence of admission ICU [2]. While a high lactate value at admission is linked to prognosis, a single lactate measurement may exhibit static variability [4]. Hence, it is advisable to assess the levels of lactate and its fluctuations during the 2nd, 6th, and 24th hours throughout research investigations [5]. Yadigaroğlu M et al. demonstrated that the measurement of lactate levels and lactate clearance (LC) within 24 hours can serve as a reliable predictor of mortality in patients with COVID-19 pneumonia [6]. Furthermore, LC has been determined to be more useful than the baseline lactate level in assessing the results of patients with sepsis and septic shock [7].
According to the literature, early risk assessment should be performed using clinical and laboratory results for pneumonia patients admitted to the ED and have a high mortality rate [8, 9]. The CURB-65 score is commonly utilized for this purpose (Confusion, Urea > 7 mmol/L, Respiratory rate ≥ 30/min, Blood pressure systolic < 90 mm Hg and/ or diastolic ≤ 60 mm Hg, Age ≥ 65 ). Although the CURB-65 score is intended to predict high-risk patients and mortality, it is particularly popular in the ED since its computation is easy in comparison to more sophisticated scores [2]. CURB-65 is a powerful prognostic indicator, however, its ability to accurately predict admission and hospital mortality is limited. Therefore, it is advised to utilize CURB-65 in conjunction with other laboratory markers [1]. Two studies done by Frenzen FS and Chen YX et al. examined the effectiveness of CURB65-L, a combination of CURB-65 and lactate, in predicting mortality and prognosis [1, 2]. Both studies found that the prediction ability of CURB65-L increased when compared to lactate and the CURB- 65 score alone. As far as we know, there has been no study undertaken to examine the ability of CURB65-LC to predict outcomes in patients with pneumonia. Hence, our study aims to examine the correlation between lactate, LC, CURB-65, CURB65-L, and CURB65-LC with mortality in pneumonia patients admitted to ED.
Materials and Methods
Study Design and Patient Population
Male and female patients over 18 years of age, who were diagnosed with pneumonia and hospitalized in the ED between 01 January and 01 May 2023, and who met the inclusion criteria, were retrospectively examined. The research comprised patients whose complete laboratory data could be retrieved from the hospital registry system and who were diagnosed with pneumonia based on current guidelines [10]. The study excluded individuals with cancer, pregnant women, individuals with a history of renal and liver illness, individuals with hospital-acquired or aspiration pneumonia, individuals with active tuberculosis, individuals with immunosuppression, and those who tested positive for PCR. The patients were categorized into risk groups based on their CURB-65 score and lactate (L1) level upon presentation to the ED. The CURB- 65 score categorizes patients into different risk levels based on their score. A score of ≤ 1 is mild, a score of 2 is moderate, and a score of ≥ 3 is considered severe risk [10]. The categorization of lactate risk was established as follows: low (lactate <2 mmol/L), intermediate (2–4 mmol/L), and high (>4 mmol/L) [2]. LC (%): [lactate at admission (L1) – lactate at 24th hour (L2) / L1) × 100] was calculated with the formula [6]. The assessment of mortality was conducted using in-hospital mortality. The study evaluated L1, LC levels, and CURB-65 scores in patients who survived and those who did not, both in the ICU and and/or in the ward. It also examined the necessity for MV and/or VS, as well as the length of hospital stay (LOHS) ≤10 days and >10 days. Furthermore, it assessed the predictive usefulness of L1, L2, LC, CURB-65, CURB 65-L, and CURB 65-LC for mortality.
Data Collection and Laboratory Tests
Age, gender, history of these patients, vital signs, lactate level in VBG (L1) and CURB-65 score at the time of admission to the ED, lactate level (L2) at the 24th hour, the clinic where they were hospitalized (ward/ ICU), whether they required MV and/or VS during their follow-up in the ICU, LOHS, and its outcomes (discharge/death) were accessed retrospectively from the hospital registry system and patient epicrisis. The urea level was measured using the Mindray chemistry analyzer BS- 2000M device (Shenzhen, China). Lactate levels were assessed using a Siemens Healthcare diagnostic Rapidpoint 500 blood gas device (Duplin, Ireland).
Statistical Analysis
Numerical parameters were expressed as median (min-max) or mean±SD, and categorical variables were expressed as frequency and percentage (%). Kolmogrov-Smirnov test, histogram analyses and skewness/kurtosis data were used to evaluate the conformity of the numerical variables to normal distribution. Levene’s test was used to analyse the intergroup homogeneity of the numerical parameters. For the comparison of two independent groups, independent t-test was used for the parameters showing normal distribution characteristics, and one-way ANOVA tests were used for the comparison of multiple groups. Mann-Witney U test was used for parameters that did not show normal distribution characteristics and Kruskal-Wallis H tests were used for comparison of multiple groups. Variables that may be associated with mortality were detailed by ROC analysis. In our study, type-I error (alpha) was taken as 0.05 (5%), p<0.05 was accepted as significant and SPSS 21.0 (IBM Inc, Chicago, IL, USA) programme was used.
Ethical Approval
This study was approved by the Ethics Committee of Necmettin Erbakan University, Faculty of Medicine (Date: 2023-06-16, No: 2023/4378(14509)).
Results
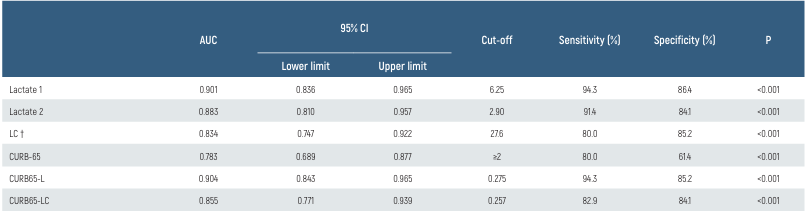
Table 1 presents a comparison of findings between surviving and non- surviving patients. Of a total of 123 patients, 88 survived, while 35 passed away. A comparison was made between surviving and non-surviving patients with regard to age, gender, and LOHS. The average age of those who died was significantly higher (p<0.01 for all). However, no significant difference was seen in terms of gender and LOHS (p=0.34, 0.45). The CURB-65 score, L1 and L2 levels, VS, and ICU admission rate were all significantly higher (p<0.001) in the non-surviving patients. In contrast, the LC and MV support rate were both significantly lower in the non-survivor group (p<0.001 for all). When comparing the L1, LC, and CURB-65 scores of patients admitted to the ICU vs those who were not, it was seen that the L1 and CURB-65 scores were significantly higher, while the LC score was lower in the ICU-admission group (p<0.001 for all). When comparing the L1, LC, and CURB-65 scores between patients who got MV support and those who did not, it was found that the L1 and CURB-65 scores were significantly higher, while the LC score was lower in the group that received MV support (p<0.001 for all). Comparing the L1, LC, and CURB-65 scores of patients who received VS with those who did not, it was discovered that the L1 and CURB-65 scores were significantly higher, while the LC score was lower in the group receiving VS (p<0.001 for all). When comparing the L1, LC, and CURB-65 scores between individuals with LOHS ≤ 10 days and LOHS >10 days, no significant difference was seen (p = 0.50, p = 0.48, p = 0.22) (Table 2). Table 3 shows a ROC analysis of L1, L2, LC, CURB-65, CURB65-L, and CURB65-LC in the mortality prediction. AUC values, sensitivity and specificity values of L1 and CURB65-L were similar. L1 and CURB65-L had the highest AUC values, while CURB-65 had the lowest AUC value (0.901, 0.904, 0.783, respectively). When the LC cut-off was 27.6, the AUC was 0.834, with 80% sensitivity and 85.2% specificity. It was determined that the AUC values of CURB65-L and CURB65-LC were greater than those of CURB-65 and LC alone (0.904, 0.855, 0.783, and 0.834, respectively) (p<0.001 for all) (Table 3). Figure 1 illustrates the risk classification distribution for the L1, CURB-65 score and CURB65-L. As a result, there was an increased mortality rate and ICU admission rate among patients with Lactate>4 (figure A) in comparison to those with CURB-65≥3 (figure B). The mortality and ICU admission rates for patients with [Lactate>4 or CURB-65≥3] (figure C) were significantly higher than those for patients with figure A or figure B alone.
Discussion
Ongoing attempts are being made to uncover risk indicators that might predict prognosis in individuals with CAP, given its high morbidity and mortality. It is advisable to categorize the level of risk in these patients before making the decision to discharge [9, 10, 11]. Several risk prediction models, such as CURB-65, and some laboratory findings have been demonstrated to be correlated with mortality in these patients [12]. Nevertheless, CURB-65 may be lacks sufficient predictive power for ICU admission and mortality [1, 11, 12]. Consequently, researchers have started to explore new prediction models that incorporate admission lactate levels for patients with CAP [1, 2, 11].
The primary factors contributing to excessive lactate production include hypoxia, alterations in mitochondrial oxidation, and glycolysis [13]. There are many studies in the literature about the prognostic power of lactate in critically ill geriatric patients, hemorrhagic shock, and trauma, where there is tissue hypoperfusion [5, 14, 15, 16]. ED often employs serum lactate levels to assess several acute medical conditions [17]. Hyperlactatemia, a laboratory finding that can be easily measured, is known to be linked with poor outcomes in critically ill patients, including the requirement for MV, admission to the ICU, and in-hospital mortality [5, 6]. The current guidelines for sepsis recommend using serum lactate as a supplementary test to establish the possibility of sepsis in these patients [18]. A study that the lactate at admission was linked to mortality in inpatients with CAP [12]. Another study highlighted that particularly elevated lactate levels should be monitored closely [1]. Chen YX et al. found that lactate levels were significantly higher in pneumonia patients who died, and these levels were able to independently predict the mortality within 28 days, as well as the probability of hospitalization and admission to the ICU (AUC: 0.823, 0.821 and 0.922, respectively) [2]. Our study revealed that levels of L1 were significantly elevated in high-risk patients who died, received MV or VS, and were admitted to the ICU, as compared to individuals with mild to moderate risk. In addition, the L1 level had a higher predictive power for mortality compared to LC and CURB-65 (AUC: 0.901, 0.834, 0.783 p<0.001). Thus, the measurement of lactate levels upon admission to the ED can effectively assist clinicians in forecasting unfavorable outcomes.
Since the sensitivity and specificity of a single lactate value is controversial, it has been stated that serial measurements over time or LC may be more reliable indicators [5, 7]. A study found that focusing on LC rather than a single lactate level would have a more significant impact on reducing mortality [19]. Yadigaroğlu M. et al. highlighted that LC levels in the 24th hour, as opposed to lactate at admission, can serve as a reliable predictor of mortality in patients with COVID-19 [6]. Sugimoto M et al. stated that LC has a poorer ability to predict outcomes in patients with pneumonia compared to those without pneumonia [7]. Cao Y. et al. observed that the levels of LC in surviving patients were higher than those in patients who had died. Furthermore, a correlation was established between decreasing LC and increasing mortality. [5]. Our study revealed that high-risk patients who died, received MV or VS, and were admitted to the ICU had lower levels of LC compared to mild-moderate risk patients. Furthermore, When the LC cut-off was 27.6, it showed a higher AUC, sensitivity and specificity in the prediction of mortality compared to CURB-65. Thus, LC levels measured at the 24-hour may serve as a more dependable prognostic indicator for these patients.
Recent studies have proven that combining risk scores such as the National Early Warning Score (NEWS) and CURB-65 with lactate and/or LC improves the prognostic performance of each parameter [5, 14, 20]. According to Jo S et al., the addition of lactate to the NEWS resulted in the creation of a new scoring system called NEWS-L. They stated that this NEWS-L demonstrated a superior capacity to predict mortality in patients with CAP compared to using either the NEWS or CURB-65 scores alone [11]. Frenzen FS et al. emphasized that additional lactate measurement in patients with low CRB/CURB-65 scores may enable detection of a deterioration of approximately 40% of the patients [1]. Chen YX et al. demonstrated that AUC values of LAC-CURB-65 in predicting 28-day mortality, hospitalization, and ICU admission were higher than those of CURB-65 alone (AUC: 0.851, 0.828, 0.955 - 0.692, 0.613, 0.710, respectively). The authors also stated that the risk classification method was capable of efficiently differentiating high- risk patients than low-risk patients [2]. The findings of our study align with those reported in the literature. In predicting mortality, CURB65-L and CURB65-LC achieved superior predictive power compared to LC or CURB-65 alone. On the basis of the risk classification model comprising lactate>4 or CURB-65≥3, it was determined that high-risk patients had a greater incidence of mortality and ICU admissions than low-risk patients. As a result, the efficacy of incorporating lactate and LC into the CURB-65 score for risk and mortality prediction will be superior to their individual utilization.
Figures

Figure 1. The risk classification distribution for the Lactate, CURB-65 score and CURB65-L
Tables
Table 1. Comparison of findings between surviving and non-surviving patients
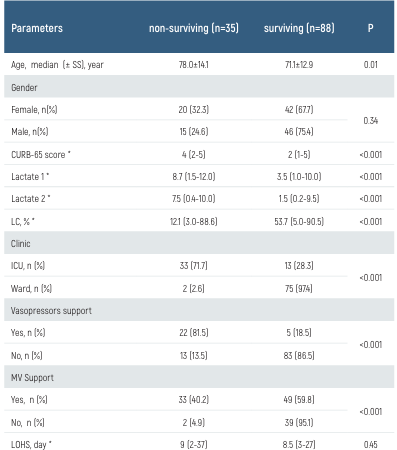
Table 2. Relationship of lactate 1, LC and CURB-65 parameters to patient groups
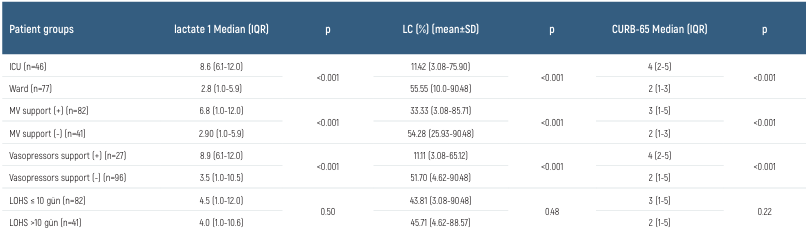
Table 3. ROC analysis of parameters in the mortality prediction
Limitations
First, our results should be corroborated by larger studies involving a greater number of patients, as this is a single-center study with a limited patient population. Second, due to the inability to conduct follow-up on the discharged patients, we were only able to report short-term mortality. Third, due to the retrospective nature and lack of double-blinding, the study was open to bias and unidentified confounding variables. Fourth, lactate levels were only measured at the time of admission to the ED and at the 24-hour mark. Additional lactate analysis (at 2nd, 6th, or 12th hours) was not feasible. Fifth, the results of our study, which primarily included geriatric patients, might have been influenced by factors such as the length of time patients were admitted to ED, the use of prescription medications, or the presence of multiple comorbid diseases. However, these circumstances were disregarded as the study was retrospective in nature.
Conclusion
On admission to the ED, the lactate, CURB-65 score, and 24th hour LC levels of patients with pneumonia may be used to predict adverse outcomes. The L1 and CURB-65 scores were found to be significantly higher in the ICU admission group that received MV and VS support. Conversely, the LC score was found to be lower in this group. Furthermore, the combination of CURB65-L and CURB65-LC enhances the predictive power of CURB-65 and LC alone in predicting mortality.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Frenzen FS, Kutschan U, Meiswinkel N, Schulte-Hubbert B, Ewig S, Kolditz M. Admission lactate predicts poor prognosis independently of the CRB/CURB-65 scores in community- acquired pneumonia. Clin Microbiol Infect. 2018;24(3):306.e1-306.e6.
-
Chen YX, Li CS. Lactate on emergency department arrival as a predictor of mortality and site-of-care in pneumonia patients:a cohort study. Thorax. 2015;70(5):404-10.
-
Kurt NG, Orak M, Üstündağ M. The role of lactate clearance on deciding discharge in exacerbation of chronic obstructive pulmonary disease: Retrospective cohort study. J Surg Med. 2018;2(2):96-8.
-
Pıhtılı A, Mammadova K, Kıyan E. Lactate Level in Stable COPD Patients. Med J SDU. 2021;28(3):427-32.
-
Cao Y, Yao S, Shang J, Ping F, Tan Q, Tian Z, et al. The combination of lactate level, lactate clearance and APACHE II score better predicts short-term outcomes in critically ill patients: a retrospective cohort study. BMC Anesthesiol. 2022;22(1):382.
-
Yadigaroğlu M, Çömez VV, Gültekin YE, Ceylan Y, Yanık HT, Yadigaroğlu NÖ, et al. Can lactate levels and lactate kinetics predict mortality in patients with COVID-19 with using qCSI scoring system?. Am J Emerg Med. 2023;66:45-52.
-
Sugimoto M, Takayama W, Murata K, Otomo Y. The impact of lactate clearance on outcomes according to infection sites in patients with sepsis: A retrospective observational study. Sci Rep. 2021;11(1):22394.
-
Eravci FC, Poyraz N, Korkmaz C, Alper H, Orhan M, Dundar MA, et al. The relationship between pneumonia severity and the presence of anosmia and ageusia in hospitalized patients with Covid-19. Selcuk Med J. 2021;37(4):339-44.
-
Küçükceran K, Ayrancı MK, Girişgin AS, Koçak S, Dündar ZD. The role of the lactate/albumin ratio in predicting mortality in COVID-19 patients in the emergency department. Mev Med Sci. 2023;3(1):5-10.
-
Metlay JP, Waterer GW. Update in adult community-acquired pneumonia: key points from the new American Thoracic Society/Infectious Diseases Society of America 2019 guideline. Curr Opin Pulm Med. 2020;26(3):203-7.
-
Jo S, Jeong T, Lee JB, Jin Y, Yoon J, Park B. Validation of modified early warning score using serum lactate level in community-acquired pneumonia patients. The National Early Warning Score–Lactate score. Am J Emerg Med. 2016;34(3):536-41.
-
Gwak MH, Jo S, Jeong T, Lee JB, Jin YH, Yoon J, et al. Initial serum lactate level is associated with inpatient mortality in patients with community-acquired pneumonia. Am J Emerg Med. 2015;33(5):685-90.
-
Pagano A, Porta G, Bosso G, Allegorico E, Serra C, Mercurio V, et al. Blood lactate in mild and moderate ARDS secondary to SARS COV 2. Am J Emerg Med. 2023;66:73-5.
-
Dundar ZD, Kocak S, Girisgin AS. Lactate and NEWS-L are fair predictors of mortality in critically ill geriatric emergency department patients. Am J Emerg Med. 2020;38(2):217-21.
-
Baxter J, Cranfield KR, Clark G, Harris T, Bloom B, Gray AJ. Do lactate levels in the emergency department predict outcome in adult trauma patients? A systematic review. J Trauma Acute Care Surg. 2016;81(3):555-66.
-
Zadorozny EV, Weigel T, Stone A, Gruen DS, Galvagno SM Jr, Yazer MH, et al. Prehospital lactate is associated with the need for blood in trauma. Prehosp Emerg Care. 2022;26(4):590- 99.
-
Kramer A, Al Agha S, Böhm L, Michael M, Schulze-Bosse K, Bernhard M. Lactate in emergency medicine. Anaesthesist. 2020;69(11):826-34.
-
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-1247.
-
Rehman F, Zafar SB, Aziz A, Aziz A, Memon PS, Ejaz T, et al. early lactate clearance as a determinant of survival in patients with sepsis: Findings from a low-resource country. J Crit Care Med (Targu Mures). 2023;9(1):30-8.
-
Donoso Calero MI, Mordillo-Mateos L, Martín-Conty JL, Polonio-López B, López-González Á, Durantez-Fernández C, et al. Modified rapid emergency medicine score-lactate (mREMS-L) performance to screen non-anticipated 30-day-related-mortality in emergency department. Eur J Clin Invest. 2023;53(8):e13994.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Necmettin Erbakan University Faculty of Medicine (Date: 2023-06-16, No: 2023/4378(14509))
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Birsen Ertekin, Tarık Acar, Alpay Tuncar, Azmi Eyiol. The relationship of CURB65-L and CURB65-LC (lactate clearance) with mortality in pneumonia patients admitted to the emergency department. Eu Clin Anal Med 2024;12(2):22-26
Publication History
- Received:
- April 6, 2024
- Accepted:
- April 29, 2024
- Published Online:
- April 30, 2024
- Printed:
- May 1, 2024
