Retrospective analysis of patients involved in intensive care for poisoning and received extracorporal treatment
Extracorporal treatment in poisoning
Authors
Abstract
Aim We planned to examine patients who presented to the emergency department with poisoning and were followed up in intensive care in terms of extracorporeal treatment.
Material and Methods The study was conducted retrospectively. Patients who were admitted to the emergency department due to poisoning between 2008 and 2018 and were followed up in intensive care and received extracorporeal treatment were included in the study.
Results 152 patients were included in the study. The median age of the included patients was 37.5 years. 88 (57.9%) of the patients were women and 64 (42.1%) were men. Of the patients participating in the study, 52 (34.2%) were on mushrooms, 29 (19.1%) were on antiepileptics, 16 (10.5%) were on methanol-ethylene glycol, 9 (6%) were on antihypertensives, and 7 were on antihypertensives. (4.5%) were tricyclic antidepressants, 6 (3.9%) were lithium, 5 (3.3%) were opioids, 3 (2%) were organophosphates, 3 (2%) were digoxin, 3 (2%) were monitored for theophylline, 3 (2%) for oral anti-diabetic, 3 (2%) for aspirin, and 3 (2%) for paracetamol. 35 (23%) required mechanical ventilation, 24 (15.8%) developed CKD after extracorporeal treatment, 20 (13.1%) developed multiorgan failure, and 20 (13.1%) developed in-hospital mortality.
Discussion It was determined that the data we obtained were compatible with the existing literature when considering the studies in the literature and current intensive care patient evaluation criteria.
Keywords
Introduction
Poisoning has been a serious public health problem since the early ages of humanity until today.Poisonings occur as a result of taking high doses of drugs or substances for suicide purposes or unintentionally. Depending on the type of substance ingested and the duration of admission to the hospital, it can have many serious consequences, including death [1]. According to the data of the World Health Organization, approximately three hundred thousand people die every year due to different poisonings [2].
Although the substances to which patients who apply to the emergency room with poisoning are exposed may differ, the basic treatment approach is common. Approach to the poisoning patient; Supportive treatment includes ensuring decontamination, increasing elimination if necessary, and antidote treatment, if available [3, 4].
In severely poisoned patients, increasing toxin elimination may improve the outcome of some poisonings [5, 6]. Extracorporeal treatment is the most appropriate treatment for the elimination of toxins with low molecular weight, low protein binding and high water solubility [7]. Examples of this include mushrooms, salicylate, theophylline, metformin, methanol, barbiturate, lithium, ethylene glycol and valproic acid [3, 7, 8].
Extracorporeal treatments (ECT) include a heterogeneous group of treatment methods that include the removal of endogenous or exogenous toxins from the body and temporarily replacing one of the vital organs [9].
In this study, we planned to evaluate patients who presented to the emergency department with poisoning and were followed up in the Intensive Care Unit in terms of the need for extracorporeal treatment.
Materials and Methods
Patients who were admitted to the emergency department due to poisoning between 2008 and 2018 and were followed up in intensive care and received extracorporeal treatment were included in our study. Patients under the age of 18 were not included in the study. Pregnant patients were also excluded from the study. Patients’ complaints, vital signs at the time of admission (Blood Pressure, Pulse, Glasgow Coma Scale, presence of hypotension), medical history (Diabetes Mellitus, Congestive Heart Failure, Chronic Renal Failure, Hypertension), blood gases (PH, pO2, pCO2, HCO3, base deficit, Lactate, Anion Gap, SID, SIG, Osmolarity, Osmolar Open), hematological (Hemoglobin, White Cell, Platelet, PT, PTT, INR) and biochemical markers (Urea, Creatinine, Potassium, Aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT), Albumin, Bilirubin, Creatinine Kinase). , Troponin) was recorded. The intoxication factor, duration of hospitalization, need for mechanical ventilation, multiorgan failure, and in-hospital mortality were recorded. The type of extracorporeal treatment the patients received, how many times they received extracorporeal treatment, urine output in the first 24 hours, whether any complications of extracorporeal treatment developed, whether CKD developed after extracorporeal treatment, and if discharged, whether they applied to the psychiatric outpatient clinic after discharge were recorded.
Statistical analysis
The analysis of the data obtained was made in the SPSS (Statistical Package for Social Science) for Windows 22.0 package program. The distribution of data was evaluated using the Kolmogorov-Smirnov test. Descriptive variables were expressed as mean ± standard deviation for normal distributions and median and IQR for non-normal distributions. To compare the means of two independent groups, the Chi-square test and/or Fisher’s exact test were used for categorical variables, and the Independent Sample t-test or Mann-Whitney U test was used for numerical variables. In addition, ROC analysis was performed to determine the sensitivity, specificity, negative and positive predictive values, general accuracy rates, and cut-off values of the study parameters, and if necessary, these analyses were optimized with Youden’s index. Values obtained as p<0.05 were considered statistically significant.
Ethical Approval
This study was approved by the Ethics Committee of Necmettin Erbakan University, Meram Faculty of Medicine Research on Non- Pharmaceutical and Medical Devices Ethics Committee (Date: 2018-06- 01, No: 2018/1400).
Results
Demographic Findings
Between 2008 and 2018, a total of 7941 patients were followed up in the intensive care units of our clinic due to poisoning. 66.4% (5269) of them were women and 33.6% (2672) were men. The median age of these patients was calculated as 24 (17) years.
152 patients were included in the study (1.9%). The median age of the patients included in the study was 37.5 (29) years. 88 (57.9%) of the patients were women and 64 (42.1%) were men. In the medical history evaluation, 31 (20.4%) of the patients had diabetes mellitus, 23 (15.1%) had heart failure, 2 (1.3%) had chronic renal failure, and 43 (28.3%) had diabetes mellitus. hypertension was present. The average pulse of those included in the study was calculated as 80±23.5. At the time of admission to the hospital, Glasgow Coma Scale (GCS) was 15 in 87 (57.2%), 13-14 in 28 (18.4%), 8-12 in 21 (13.9%), 4-7 in 15 (9.9%). It was evaluated as 3 in 1 (0.6%). Hypotension was present in 38 (24.3%) of the patients (Table 1).
Of the patients participating in the study, 52 (34.2%) were on mushrooms, 29 (19.1%) were on antiepileptics, 16 (10.5%) were on methanol-ethylene glycol, 9 (6%) were on antihypertensives, and 7 (4.5%) were on antihypertensives. ) tricyclic antidepressant, 6 (3.9%) lithium, 5 (3.3%) opioids, 3 (2%) organophosphates, 3 (2%) digoxin, 3 (2%) theophylline, 3 (3%) (2%) were followed up for oral anti-diabetic use, 3 (2%) for aspirin, and 3 (2%) for paracetamol (Table 2).
Mean and median [4] values of the patient’s blood gas parameters: pH 7.34 (0.12), pO2 46.5 (27) mmHg, pCO2 37.6±10.5 mmHg, HCO3 20±5.82mmol/lt, Base Deficit -4.45(7) mmol/lt, Osmolarity 289.31±11.53mmol/kg, Osmolar Deficit 2.81±8.99 mmol/kg, Lactate 1.8(3) mmol/lt, SID 33±4.95, SIG was calculated as -1.9±7.57, Anion Open was calculated as 11.55±7.42 (Table 1). The median hospital stay of the patients was evaluated as 5 (4) days. As an extracorporeal treatment option, 85 (55.9%) preferred hemodialysis, 7 (4.6%) ultrafiltration, 31 (20.4%) hemoperfusion, and 29 (19.1%) carbon filters. The median number of extracorporeal treatment sessions of these cases was calculated as 1(1). After extracorporeal treatment, the median 24-hour urine output was measured as 2500 (3400) ml. Extracorporeal treatment complications developed in 4 (2.6%) cases. 35 (23%) required mechanical ventilation, 24 (15.8%) developed CK despite extracorporeal treatment, 20 (13.1%) developed multiorgan failure, and 20 (13.1%) developed in-hospital mortality; 53 (34.8%) of them applied to the psychiatric outpatient clinic after discharge.
Relationship between Obtained Data and In-Hospital Mortality
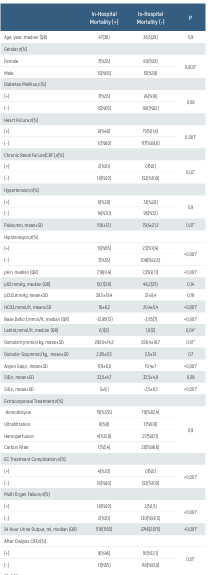
When the patients included in the study were compared in terms of age and in-hospital mortality, the median age of the patients with in hospital mortality was calculated as 47(36) while the median age of the patients without in-hospital mortality was calculated as 36.5(29). It was not statistically significant (p>0.05). When gender and in-hospital mortality were compared, in-hospital mortality was found to be 8% in women and 20% in men (p=0.003).
When comorbidities and in-hospital mortality were compared, heart failure and chronic renal failure were statistically significant in terms of in-hospital mortality and p-values were calculated as 0.001 and 0.02, respectively (Table 3).
When the presence of hypotension at the time of admission to the hospital was compared with in-hospital mortality, 65% of the patients with in-hospital mortality had hypotension. Only 17.4% of the patients with no in-hospital mortality had hypotension (p<0.0001). The average pulse rate of patients with in-hospital mortality on admission to the hospital was calculated as 100±31.1, and the average pulse rate during admission of patients without in-hospital mortality was calculated as 79.5±21.2 (p=0.01) (Table 3).
When in-hospital mortality and blood gas analysis at admission were compared, pH, HCO3, Base Deficit, Lactate, Osmolarity, Anion Deficit, SIG were found to be statistically significant. (p<0.05) (Table 3). A statistically significant relationship was found between extracorporeal treatment complications, development of multiorgan failure, 24-hour urine output after extracorporeal treatment, and in-hospital mortality (p<0.05) (Table 3).
Relationship between Obtained Data and the Need for Mechanical Ventilators
When the patients were compared in terms of age and need for mechanical ventilators, the median age of the patients who needed a mechanical ventilator was calculated as 40 (3), while the median age of the patients who did not need a mechanical ventilator was calculated as 35 (29). It was not statistically significant (p>0.05). When gender and mechanical ventilator needs were compared, the need for mechanical ventilators was found to be 16.1% in women and 32.8% in men (p = 0.02). When the presence of comorbidities and the need for mechanical ventilators were compared, the presence of heart failure was found to be significant in terms of mechanical ventilator need. (p<0.05).
While the average pulse rate of patients requiring mechanical ventilation was calculated as 94±28.9, the average pulse rate for mechanical ventilators was calculated as 82.5±21 (p<0.05). While hypotension was detected in 45.7% of the patients who needed mechanical ventilation, only 17.1% of the patients who did not need a ventilator had hypotension (p<0.0001).
When blood gas analysis and mechanical ventilator requirement were compared, pH, HC03, Base Deficit, Lactate, Osmolarity, Osmolar Deficit, SID, and SIG were statistically significant. (p<0.05). When hematological examinations and mechanical ventilator requirements were compared, white blood cell count, aPTT, and INR were found to be statistically significant. It was found to be statistically significant (p<0.05). When biochemical parameters were evaluated in terms of mechanical ventilation needs, glucose, urea, creatinine, potassium, AST, CK, and Troponin I were calculated to be statistically significant (p<0.05). Among the patients included in the study, the median (IQ) hospitalization period of the patients who required mechanical ventilation was 5(7) days, while the median hospitalization duration of the patients who did not require mechanical ventilation was calculated as 5(3) days (p>0.6). The need for mechanical ventilation and the type of extracorporeal treatment, the presence of extracorporeal treatment complications, the development of multiorgan failure, 24-hour urine output after extracorporeal treatment, and the development of CKD after extracorporeal treatment were statistically significant in the patients who continued to study (p<0.05).
The Relationship betweeen Obtained Data and the Development of Chronic Renal Failure
While the median age value of patients who developed chronic renal failure despite extracorporeal treatment was 48 (40), the median age value of patients who did not develop chronic renal failure was found to be 35 (29) (p<0.05). While 33.3% were female, 66.7% were male (p<0.05) when the presence of additional diseases and the development of Chronic Renal Failure after extracorporeal treatment were compared, the presence of Diabetes Mellitus, Heart Failure, Chronic Renal Failure, and Hypertension was found to be statistically significant (p<0.05).
When blood gas analysis and the development of Chronic Renal Failure after extracorporeal treatment were compared, pH, HCO3, Lactate, Osmolarity, Anion Open, SID, and SIG were evaluated as statistically significant (p <0.05). When hematology laboratory findings and the development of Chronic Renal Failure after extracorporeal treatment were compared, any value was not significant. (p>0.05). When biochemical parameters were compared with the development of Chronic Renal Failure after extracorporeal treatment, urea, creatinine, sodium, potassium, albumin, and CK values were statistically significant (p<0.05).
While 45% of the patients who developed multiorgan failure during treatment developed Chronic Renal Failure after extracorporeal treatment, only 12.1% of the patients who did not develop multiorgan failure developed Chronic Renal Failure after extracorporeal treatment (p<0.0001).
ROC Analyzes to Predict Mortality
The performance characteristics of osmolarity in predicting mortality (area under the curve, sensitivity, specificity, predictive value, and likelihood ratios) were calculated. The cut-off value obtained using the ROC curve for mortality was 305.75 (sensitivity: 35%, specificity: 94.7%, area under the curve: 0.67, 95% confidence interval: 0.59-0.74, p: 0.02) (Figure 1).
The performance characteristics of the SIG value in predicting mortality (area under the curve, sensitivity, specificity, predictive value, and likelihood ratios) were calculated. The cut-off value obtained using the ROC curve for mortality was 16 (sensitivity: 25%, specificity: 99.24%, area under the curve: 0.76, 95% confidence interval: 0.69-0.83, p:< 0.0001) (Figure 2)
Discussion
Poisonings constitute a significant portion of emergency room visits. In severely poisoned patients, increasing toxin elimination may improve the outcome of some poisonings.[8] In our study, we retrospectively examined patients who presented to the emergency department with poisoning and received extracorporeal treatment.
In a study conducted by Lund C. et al., where acute poisonings were evaluated throughout Oslo, 117 of 912 toxicology cases died, 88 (75%) of which were male and 29 (25%) were female, and the median age was 41 (29-51). It has been determined that. In the same study, 8 patients died during their hospitalization. Of these patients, 6 were female and 2 were male, and the median age was determined to be 42 (29) years.[10] In our study, it was determined that the median age of the 152 patients requiring hemodialysis included in the study was 37.5 (29) years old, 88 (57.9%) of the patients were female and 64 (42.1%) were male. Again, when examined in terms of mortality; While the median age of patients with in-hospital mortality was 47 (36), the median age of patients without in-hospital mortality was calculated as 36.5 (29). However, no significant relationship was detected between mortality and age. When the relationship between gender and in-hospital mortality is examined; Contrary to the study of Lund C. et al., it was determined that in patients admitted to intensive care and requiring hemodialysis, the mortality rate was higher in men (male = 20%, female = 8%) and there was a significant relationship between gender and in-hospital mortality (p = 0.003).
When the current literature is examined in terms of poisoning types and the need for extracorporeal treatment; The study of Mardini J. et al. is a remarkable study on this subject. In the relevant study, 2908 patients who received extracorporeal treatment between 1913 and 2014 were examined. When the study data were examined, it was determined that methanol, ethylene glycol, salicylate, lithium and theophylline poisonings were generally more common, although their frequency varied in each decade [11]. In our study, when the data of 152 patients receiving extracorporeal treatment were examined, it was determined that mushroom poisoning ranked first with a rate of 34.2%. This is followed by antiepileptic drugs with a rate of 19.1%, and methanol and ethylene glycol poisoning with 10.5%. Methanol and ethylene glycol are among the top three, according to Mardini et al. is similar to his work.
In cases of poisoning, patients’ vitals and laboratory findings at the time of admission are important issues in clinical evaluation. In a study by Lee et al examining 1512 poisoning cases over a 1-year period. 63 of the cases were classified as fatal poisonings and deaths occurred. 9 of the patients died during transportation to the emergency room, 2 died in the emergency room and 52 died while hospitalized. When these data are examined; Parameters such as male gender, being over 60 years of age, abnormal heart rhythm (tachycardia heart rate > 120/min or bradycardia heart rate < 60/min), low GCS, hypotension, respiratory failure, and having an additional disease are determining factors for mortality. It has been concluded [12]. In our study, 65% of the patients who developed in-hospital mortality were male, and it was determined that men needed mechanical ventilation more than women, with a rate of 32.8%. Again, when hypotension was examined, it was determined that 65% of the patients who developed in-hospital mortality, as well as 45.7% of the patients who required mechanical ventilation, were hypotensive. A significant relationship was found between the presence of hypotension and in-hospital mortality and the need for mechanical ventilation (p<0.05). Again, in our study, when the relationship between the presence of comorbidities and mortality and the need for mechanical ventilation was examined, it was determined that in-hospital mortality levels were significantly higher in patients with concomitant heart failure and chronic renal failure (p<0.05). Additionally, the presence of heart failure was found to be significant in terms of mechanical ventilation need (p<0.05).
Laboratory parameters are one of the most important parameters used in evaluating poisoning cases. In a study conducted by Eizadi Mood et al., in 93 patients who developed coma as a result of drug poisoning, APACHE 2 scores (temperature, mean arterial pressure, heart rate, respiratory rate, oxygenation, arterial pH, serum sodium, serum potassium, serum creatinine, hematocrit, white blood cell count and Glasgow coma scale) were examined and no significant relationship was found [13].
Again, in a study by Liisananti JH et al. examining in-hospital mortality and intensive care unit stays in acute drug poisoning, they concluded that the presence of conditions such as acidosis, leukocytosis, thrombocytopenia, hyperkalemia, renal failure, hypotension, and respiratory failure increased the intensive care unit stay and in- hospital mortality.[14] In our study, when in-hospital mortality and blood gas analysis at admission were compared, a significant relationship was detected between parameters such as pH, HCO3, Base Deficit, Lactate, Osmolarity, Anion Open, SIG and mortality (p<0.05). Again, a significant relationship was detected between the elevations of white blood cells, PT, aPTT and INR, which are hematological tests, and in- hospital mortality and the need for mechanical ventilation (p<0.05). When compared with biochemical parameters, glucose, urea and creatinine. It was determined that potassium, AST, ALT and CK elevations were significant in terms of mortality and mechanical ventilator need (p<0.05). Our study data are similar to the results obtained by Liisanantti JH et al. Our study results do not coincide with the results of Eizadi Mood et al.’s study. However, poisonings such as mushroom, organophosphate and methyl alcohol, which were included in our study, were not included in the relevant study. We think that the difference in results between the two studies is due to this.
Kidney damage that develops after poisoning is an important issue that should not be ignored. In a 2015 study by Lee et al., organophosphate poisonings were collected from a cohort of 9,966 patients whose national databases were scanned. According to the results of this study, it has been shown that the risk of developing kidney damage is 1.39 times higher in patients with organophosphate poisoning, and the risk of developing kidney damage is 43.7 times higher in patients with organophosphate poisoning and requiring mechanical ventilation [15]. In our study, we examined the relationship between the need for mechanical ventilation and the type of extracorporeal treatment, the presence of extracorporeal treatment complications, the development of multiorgan failure, 24-hour urine output after extracorporeal treatment, and the development of CKD after extracorporeal treatment, and a significant relationship was found between these parameters (p<0.05).
In our study, it was found that 45% of the patients who developed multiorgan failure after poisoning developed CKD despite extracorporeal treatment, and the development of multiorgan failure and CKD after extracorporeal treatment was more common in those with additional diseases (p<0.05). It was determined that the data we obtained were compatible with the existing literature when considering the studies in the literature and current intensive care patient evaluation criteria.
Figures

Figure 1. ROC Analysis in Terms of Predicting Mortality with Osmolarity

Figure 2. ROC Analysis for Mortality Prediction with SIG
Tables
Table 1. Demographic Data
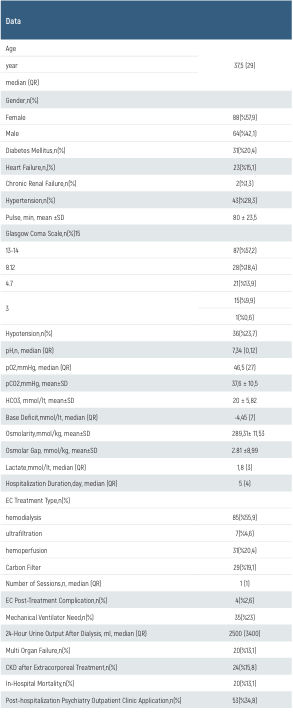
Table 2. Causes of Intoxication
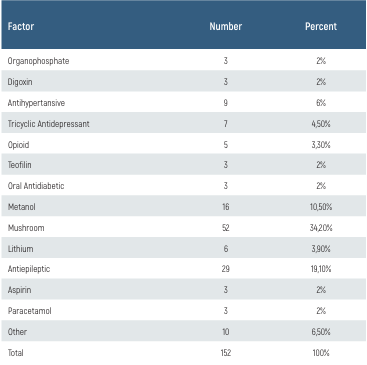
Table 3. The Relationship between Obtained Data and In-Hospital Mortality
Conclusion
Poisoning cases continue to be a serious public health problem today, as they are a significant cause of mortality and morbidity. We examined patients who were admitted to the emergency department due to poisoning between 2008 and 2018 and were followed in the Intensive Care Unit and received extracorporeal treatment. The majority of patients receiving treatment were women (57.9%). Mushroom, methanol and antiepileptics were found to be the most common causes of poisoning (34.2%-19.1%-10.5%). The preferred type of extracorporeal treatment in most patients was hemodialysis (55.9%). Extracorporeal treatment complications developed in 4 patients (2.6%) and mechanical ventilation was required in 35 patients (23%). CKD developed despite extracorporeal treatment in 24 patients (15.8%) and in-hospital mortality occurred in 20 patients (13.1%). 53 patients applied to the psychiatric outpatient clinic after discharge (34.8%).
The patients’ hypotension, tachycardism and being male at the time of admission to the hospital were found to be associated with mortality and the need for mechanical ventilation (p<0.05). Evaluation of vital signs during admission to the emergency department is very important in predicting mortality and the need for mechanical ventilation. Likewise, blood gas, hematological and biochemical parameters at admission are extremely important in predicting mortality. It was also observed that the SIG value was associated with mortality. Despite extracorporeal treatment, the development of CKD was found to be associated with higher age and the presence of comorbidities. The relationship between the development of CKD in patients with high renal function tests at admission was found to be significant (p<0.05).
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Ayaz T. Evaluation Of Drug Poisoning For Suicidal Purposes. Konuralp Medical Journal. 2015;7(1):53-56.
-
Selçuk M, Çakar N. Single Center Source Acute Poisoning Analyzes: Six Years of Case Data. Turkish Intensive Care Association Journal. 2015;13:57-61.
-
Kulig K, John M, Hockberger R, Walls R. Rosen’s Emergency Medicine-Concepts and Clinical Practice E-Book: 2-Volume Set. Elsevier Health Sciences. 2013.p.1954-1960.
-
Thompson TM, Theobald J, Lu J, Erickson TB. The general approach to the poisoned patient. Disease-a-Month. 2014;60(11):509-524.
-
Mokhlesi B, Leiken JB, Murray P, Corbridge TC. Adult toxicology in critical care: Part I: General approach to the intoxicated patient. Chest. 2003;123(2):577-592.
-
Eaton DL. CD Klaassen, editors. Principles of toxicology. Casarett and Doull’s Toxicology: The Basic Science Of Poisons. 2001.p.5-19.
-
Lavergne V, Nolin TD, Hoffman RS, Roberts D, Gosselin S, Goldfarb DS, et al. The EXTRIP (extracorporeal treatments in poisoning) workgroup: Guideline methodology. Clinical Toxicology. 2012;50(5):403-413.
-
Boyle JS, Bechtel LK, CP Holstege Management of the critically poisoned patient. Scandinavian journal of trauma, resuscitation and emergency medicine. 2009;17:1-11.
-
Ouellet G, Bouchard J, Ghannoum M, Decker BS. Available extracorporeal treatments for poisoning: Overview and limitations. In Seminars in Dialysis. Wiley Online Library. 2014;27(4):342-349.
-
Lund C, Teige B, Drottning P, Stiksrud B, Rui TO, Lyngra M, et al. A one-year observational study of all hospitalized and fatal acute poisonings in Oslo: Epidemiology, intention and follow-up. BMC public health. 2012;12:1-10.
-
Mardini J, Lavergne V, Roberts D, Ghannoum M. Case reports of extracorporeal treatments in poisoning: Historical trends. In Seminars in Dialysis. Wiley Online Library. 2014;27(4):402- 406.
-
Lee HL, Lin HJ, Yeh STY, Chi CH, Guo HR. Presentations of patients of poisoning and predictors of poisoning-related fatality: Findings from a hospital-based prospective study. BMC Public health. 2008;8:1-9.
-
Mood NE, Sabzghabaee AM, Khalili-Dehkordi Z. Applicability of different scoring systems in outcome prediction of patients with mixed drug poisoning-induced coma. Indian journal of anaesthesia. 2011;55(6):599-604.
-
Liisanantti JH, Ohtonen P, Kiviniemi O, Laurila JJ, T I Ala-Kokko. Risk factors for prolonged intensive care unit stay and hospital mortality in acute drug-poisoned patients: An evaluation of the physiologic and laboratory parameters on admission. Journal of critical care. 2011;26(2):160-165.
-
Lee FY, Chen WK, Lin CL, Lai CY, Wu YS, Lin IC, et al. Organophosphate poisoning and subsequent acute kidney injury risk: A nationwide population-based cohort study. Medicine. 2015;94(47):e2107.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Necmettin Erbakan University, Meram Faculty of Medicine Research on Non-Pharmaceutical and Medical Devices Ethics Committee (Date: 2018-06-01, No: 2018/1400)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Muhammed Kamiloğlu, Ramazan Köylü, Öznur Köylü, Fatih Emin Vişneci, Nazire Belgin Akıllı, Ozan Özelbaykal. Retrospective analysis of patients involved in intensive care for poisoning and received extracorporal treatment. Eu Clin Anal Med 2024;12(2):27-32
Publication History
- Received:
- April 19, 2024
- Accepted:
- April 30, 2024
- Published Online:
- April 30, 2024
- Printed:
- May 1, 2024
