Maternal absence in the neonatal intensive care unit during the pandemic: Can maternal scent mimic kangaroo mother care for preterm infants?
Maternal scent vs. Kmc in nicu during pandemic
Authors
Abstract
Aim To evaluate the effectiveness of maternal scent (MS) in reducing stress levels in preterm infants admitted to the Neonatal Intensive Care Unit (NICU) during restricted maternal visitation and compare its impact with Kangaroo Mother Care (KMC).
Material and Methods A total of 135 preterm infants born between 28–37 weeks of gestation, with a birth weight of 1000–2500 grams, and a 1-minute APGAR score of ≥7 were included. Infants were randomized into three groups: The Control Group was standard care without maternal contact. The MS Group was exposure to maternal scent through the mother’s undershirt for 15 days. The KMC Group was Daily Kangaroo Mother Care for 60 minutes for 15 days. Primary outcomes included serum cortisol levels, oxygen saturation, heart rate, respiratory rate, and COMFORT scores measured at baseline (Day 7) and post-intervention (Day 15).
Results On Day 15, significant differences were observed among the groups (p<0.01). The KMC group demonstrated the greatest improvements in oxygen saturation (96.87 ± 1.34), heart rate (144.23 ± 4.01 bpm), respiratory rate (42.12 ± 2.74 breaths/min), serum cortisol levels (9.87 ± 1.78 μg/dL), and COMFORT scores (12.45 ±
2.08). The MS group also showed significant improvements compared to the control group but to a lesser extent
(p<0.05). The control group displayed minimal changes across all parameters.
Discussion KMC remains the most effective intervention for reducing stress in preterm infants in the NICU. However, maternal scent exposure serves as a viable alternative to KMC when direct maternal contact is not feasible, providing significant reductions in stress markers and improving physiological stability.
Keywords
Introduction
The majority of preterm infants spend their first weeks of life in the Neonatal Intensive Care Unit (NICU), an environment vastly different from the womb, where they are exposed to various stress-inducing stimuli, such as noise, light, and painful procedures. These early-life stressors can cause long-term neurodevelopmental, emotional, and physiological problems. Preterm birth disrupts normal brain maturation, putting infants at a considerable risk of neurological vulnerability, as the brain volume increases nearly threefold during the third trimester. However, premature infants face difficulties processing external stimuli, which trigger neuroendocrine stress responses, including increases in respiration rate, heart rate, and blood pressure, further impairing brain development 1,2,3.
Premature delivery can be a stressful and traumatic experience for parents, which may have a negative impact on natural establishment of the parent-infant relationship. The NICU environment disrupts parental involvement in infant care and jeopardizes the bonding process between parents and the baby 2. Maternal scent (MS) has emerged as a non-pharmacological alternative to mitigate stress in preterm infants. Olfactory cues are vital in mammalian bonding and social attachment, as the perception of maternal scent can soothe infants, reduce crying, and trigger feeding behaviors 4. Research demonstrates that maternal scent exposure can regulate infants’ stress responses by stabilizing physiological parameters, including heart rate and oxygen saturation, and reducing cortisol levels 5,6. Although there are numerous studies highlighting the benefits of MS for preterm infants, there is a lack of comparative studies on whether MS transfer can be used in place of kangaroo care for preterm infants 5,6. As such, we sought to determine whether maternal scent, which is essential for mother-infant attachment, can be used as an alternative to kangaroo mother care in the NICU setting.
This study aimed to evaluate the impact of maternal scent (MS) and Kangaroo Mother Care (KMC) on reducing stress in preterm infants during the COVID-19 pandemic when maternal presence in neonatal intensive care units (NICUs) was restricted.
Materials and Methods
This randomized controlled clinical study followed the CONSORT guidelines and the EQUATOR Network checklist for transparency. A flowchart (Figure 1) was used to track patient selection and group allocation. The study assessed the effects of Kangaroo Mother Care (KMC) and Maternal Scent (MS) on toxic stress levels in preterm infants. Conducted at Anka Hospital NICU (Gaziantep, Turkey), the sample size was estimated using Jamovi 1.8, requiring 30 infants per group to achieve 0.7 power at a = 0.05. The study enrolled 135 preterm infants (45 per group). Administrative permissions were obtained, and written informed consent was provided by parents. The study is registered on clinicaltrials.gov (NCT05607706).
Preterm infants (28–37 weeks, 1,000–2,500 g birth weight, APGAR ≥7) hospitalized in the NICU for ≥15 days were included. Exclusion criteria included feeding problems, congenital defects, sepsis, or conditions affecting the hypothalamic-pituitary-adrenal (HPA) axis. Infants requiring mechanical ventilation, CPAP, or prior exposure to analgesics/ sedatives were also excluded. KMC eligibility was determined by a neonatal specialist, and mothers with mental or physical limitations preventing KMC were excluded.
During the COVID-19 pandemic, strict NICU isolation policies prevented maternal contact. Therefore, only Control (Group 1) and the Maternal Scent (Group 2) were initially included. Randomization used a random number table, allocating 45 infants each to these groups.
After restrictions were eased, KMC (Group 3) was introduced. The first 45 preterm infants meeting the inclusion criteria during this period were enrolled.
A total, 135 infants were included, while 43 were excluded (Figure 1). Study data were collected using the Newborn Data Form developed by the researchers 7, the Turkish adaptation of the COMFORT scale 8, and serum cortisol level measurements. The Newborn Data Form recorded sex, gestational age, birth weight, APGAR scores, diet, oxygen saturation (O2), heart rate, respiratory rate, and maternal demographics. The COMFORT scale, validated for preterm infants, assesses seven parameters on a 5-point Likert scale (higher scores indicate lower comfort). Its Cronbach’s alpha was 0.85, confirming reliability 9.
Between January and November 2021, routine blood samples were collected at Days 7 and 15 (06:00–06:30) and analyzed using chemiluminescence immunoassay. Vital signs were monitored hourly, with oxygen saturation measured via Nihon Kohden Life Scope, respiratory rate observed over 1 minute, and heart rate assessed by using a stethoscope. The COMFORT scale was scored during feeding times (08:00–10:00).
• Control Group: Standard NICU care for 15 days, with vital signs, cortisol, and COMFORT scores recorded at Days 7 and 15.
• Maternal Scent (MS) Group: Infants were exposed to mothers’ worn undershirts, washed fragrance-free and changed daily for 15 days.
• Kangaroo Mother Care (KMC) Group: Daily 60-minute skin-to-skin contact under NICU nurse supervision for 15 days.
After data collection, mothers were supported to continue KMC independently.
Statistical analysis
Data were analyzed using SPSS version 27 (IBM Corp., Armonk, NY). Normality was assessed with the Kolmogorov-Smirnov and Shapiro- Wilk tests. As variables were non-normally distributed (p < 0.05), nonparametric tests were used. The Kruskal-Wallis test compared groups, while the Wilcoxon Signed-Rank test assessed within-group changes (Day 7 vs. Day 15). Categorical variables were analyzed using the chi-square test. Pairwise comparisons were conducted with the Mann-Whitney U test and Bonferroni correction. Non-parametric ANCOVA (Quade’s test) adjusted for baseline differences. Statistical significance was set at p < 0.05, with results reported as median (IQR) for continuous variables and frequencies (%) for categorical variables.
Ethical approval
This study was approved by the Ethics Committee of Sanko University Faculty of Medicine in Gaziantep, Turkey (Date: 2020-01-15, No: 2020/15). Additionally, administrative permissions were obtained from the managers of the hospital where the research was conducted. Written informed consent was obtained from the parents of the infants after explaining them the study purpose, scope and procedures. The study was registered at ClinicalTrials.gov (NCT05607706). All participants provided voluntary written informed consent.
Results
The general characteristics of preterm infants and their mothers are presented in Table 1. There were no statistically significant differences between the groups in terms of all variables (p>0.05) (Table 1).
Table 2 shows the comparison of stress and physiological parameters among the groups at Days 7 and 15. COMFORT scores were significantly reduced in the KMC group (12.45 ± 2.08) compared to the MS group (15.78 ± 2.34) and the control group (19.34 ± 2.89) (p < 0.001). Pairwise comparisons revealed that both the MS and KMC groups showed significant improvements compared to the control group for all parameters on Day 15 (p < 0.05). The KMC group demonstrated the greatest improvements, followed by the MS group (Table 2.).
Table 3 summarizes the within-group comparisons of stress and physiological parameters between Day 7 and Day 15. The MS group demonstrated significant cortisol reduction compared to the control group (p=0.003), although KMC remained the most effective intervention (Table 3).
In terms of the between-group comparisons of the stress and physiological parameters on Day 15, significant differences were observed across all parameters among the three groups (p < 0.001 for all). The oxygen saturation was highest in the Kangaroo Mother Care (KMC) group (96.87 ± 1.34), followed by the Maternal Scent (MS) group (94.73 ± 1.67), and lowest in the Control group (92.51 ± 2.01). Pairwise comparisons revealed that the KMC group had significantly higher oxygen saturation levels than both the MS and Control groups (p < 0.001), and the MS group also showed significantly higher levels compared to the Control group (p = 0.005).
The heart rate was lowest in the KMC group (144.23 ± 4.01 bpm), followed by the MS group (150.87 ± 4.54 bpm), and highest in the Control group (154.11 ± 5.23 bpm). Pairwise comparisons showed that the KMC group had a significantly lower heart rate compared to both the MS (p < 0.001) and Control groups (p < 0.001). The MS group also had a significantly lower heart rate compared to the Control group (p = 0.012).
For the respiratory rate, the KMC group exhibited the lowest value (42.12 ± 2.74 breaths/min), followed by the MS group (47.43 ± 2.98 breaths/ min) and the Control group (50.11 ± 3.12 breaths/min). The KMC group showed significantly lower respiratory rates compared to both the MS (p < 0.001) and Control groups (p < 0.001), while the MS group had significantly lower rates compared to the Control group (p = 0.007). The serum cortisol levels were the lowest in the KMC group (9.87 ± 1.78 μg/dL), followed by the MS group (12.34 ± 2.01 μg/dL), and highest in the Control group (15.67 ± 2.45 μg/dL). The MS group also showed significantly lower cortisol levels compared to the Control group (p = rate, an increase was observed in the control and MS groups on Day 15 compared to Day 7, while the KMC group exhibited a significant decrease. The difference in heart rate changes between Days 7 and 15 was statistically significant (F (2, 92) = 9.028, p < 0.01). The magnitude of change ranked the groups as KMC < MS < Control, with the KMC group showing the greatest reduction in heart rate and the control group the least. Regarding respiratory rates, a significant difference was found among the groups when comparing Days 7 and 15 (KWH (2, 92), X2 = 57.506, p < 0.01).
For serum cortisol levels, the KMC group showed a greater reduction on Day 15 compared to Day 7, while the control and MS groups exhibited smaller decreases. The Quade test confirmed that the differences among the groups were statistically significant (p < 0.05). Pairwise analysis revealed that the difference primarily occurred between the control and KMC groups. Finally, examining changes in COMFORT scores between Days 7 and 15, a slight reduction was observed in the control group, an increase in the MS group, and almost no change in the KMC group. However, the Quade test indicated no statistically significant differences among the groups in COMFORT scores between Days 7 and 15 (p > 0.05, Figure 2).
Discussion
This study evaluated the stress levels of preterm infants in the NICU due to maternal separation, the stress-reducing effects of Kangaroo Mother Care (KMC), and the potential of maternal scent as a soothing intervention when KMC is not feasible. The findings confirmed that KMC significantly reduced stress in preterm infants, as evidenced by improvements in physiological parameters —oxygen saturation, heart rate, respiratory rate)— and reductions in serum cortisol levels and COMFORT scores. Maternal scent, while less effective than KMC, also showed a significant positive impact, suggesting it can serve as an alternative to KMC in mitigating infant distress. The study supports the hypothesis that continuous exposure to maternal scent is associated with reductions in stress biomarkers and improved physiological stability. These results highlight the importance of both interventions in NICU settings to mitigatethe adverse effects of maternal separation on preterm infants, emphasizing the need for individualized care strategies when direct maternal presence is not possible.
In recent years, advances in medical technology have significantly increased the survival rates of preterm infants, including those born as early as 23–24 weeks of gestation. However, the physical separation of infants from their mothers during NICU care remains a major challenge, contributing to adverse outcomes such as impaired neurodevelopment, maladaptive cognition, learning difficulties, and emotional and behavioral problems 3,10. Elevated stress levels, indicated by increased serum cortisol levels, have been widely reported in preterm infants experiencing maternal deprivation, with cortisol levels found to be two to four times higher in such infants 11,12.
Kangaroo Mother Care (KMC) is recognized as a simple, cost- effective intervention that reduces stress and promotes physiological stability in preterm infants by providing skin-to-skin contact. The underlying mechanism involves sensory nerve pathways that optimize neurosensory development and stabilize vital signs such as oxygen saturation, respiratory rate, and heart rate. KMC also lowers cortisol levels, shortens hospital stays, improves breastfeeding, and enhances neurodevelopmental outcomes 13,14,15. Studies have further demonstrated that KMC reduces pain associated with invasive procedures and decreases the risk of infections in preterm infants 16,17. In our study, preterm infants receiving KMC exhibited significantly lower stress levels, as evidenced by improvements in physiological parameters and reduced cortisol levels, compared to infants deprived of maternal contact.
Studies have also shown that maternal scent or breast milk scent reduces pain and stress associated with painful NICU procedures and improves vital signs such as oxygen saturation, heart rate, and blood pressure 18,19. Furthermore, maternal scent exposure has been associated with faster weight gain and reduced stress following painful procedures in preterm infants 20. Consistent with these findings, our study demonstrated that preterm infants exposed to maternal scent for an extended period (15 days) achieved significant reductions in stress levels compared to the control group.
While maternal scent exposure effectively reduced stress, cortisol levels in the MS group remained higher than those in the KMC group, reinforcing the superior benefits of KMC through direct skin-to-skin contact. Nonetheless, maternal scent serves as a valuable alternative when maternal presence through KMC cannot be achieved. Reducing stress in preterm infants is critical to mitigating its adverse effects on the cardiovascular, respiratory, endocrine, and neurological systems, particularly in the hippocampus, a region vulnerable to elevated glucocorticoid levels 20,21.
This study is unique in its evaluation of the soothing effects of maternal scent over an extended period (15 days), providing robust evidence for its efficacy in reducing stress among preterm infants. Future research should focus on the long-term neurodevelopmental and behavioral effects of maternal scent exposure and its combined use with KMC to optimize outcomes for preterm infants in NICU settings. Exposure to maternal scent shortly after birth can effectively reduce stress caused by maternal separation in the NICU and help mitigate potential long- term health complications in preterm infants. KMC remains the most effective and practical method for alleviating distress, and its initiation as early as possible after birth is crucial. However, in circumstances where mother-infant bonding cannot be achieved—such as during pandemics, natural disasters, or maternal physical limitations— maternal scent can serve as a valuable alternative. Providing maternal scent to preterm infants mimics maternal presence and has a calming effect, which is essential for preventing stress from escalating to toxic levels.
Recent systematic reviews and meta-analyses have reinforced the benefits of KMC in reducing stress and improving physiological stability in preterm infants. Studies have demonstrated that KMC not only enhances oxygenation and stabilizes vital signs but also significantly lowers cortisol levels, a key biomarker of stress. A meta-analysis by Boundy et al. highlighted the consistent reduction in neonatal morbidity and mortality with KMC application, supporting its role as an essential intervention in NICU settings 13. Additionally, research on the effects of maternal scent on cortisol regulation in neonates has provided valuable insights. Studies suggest that maternal scent exposure leads to lower cortisol levels and improved autonomic stability, reinforcing its potential as a non-invasive alternative when direct maternal contact is not possible. A pilot study by Maayan-Metzger et al. demonstrated that preterm infants continuously exposed to maternal breast milk odor exhibited significantly reduced stress parameters 20. These findings align with our study, suggesting that maternal scent can serve as a viable substitute for KMC when maternal presence is restricted. Future studies should further explore the synergistic effects of combining KMC and maternal scent exposure to optimize stress reduction in preterm infants.
Figures
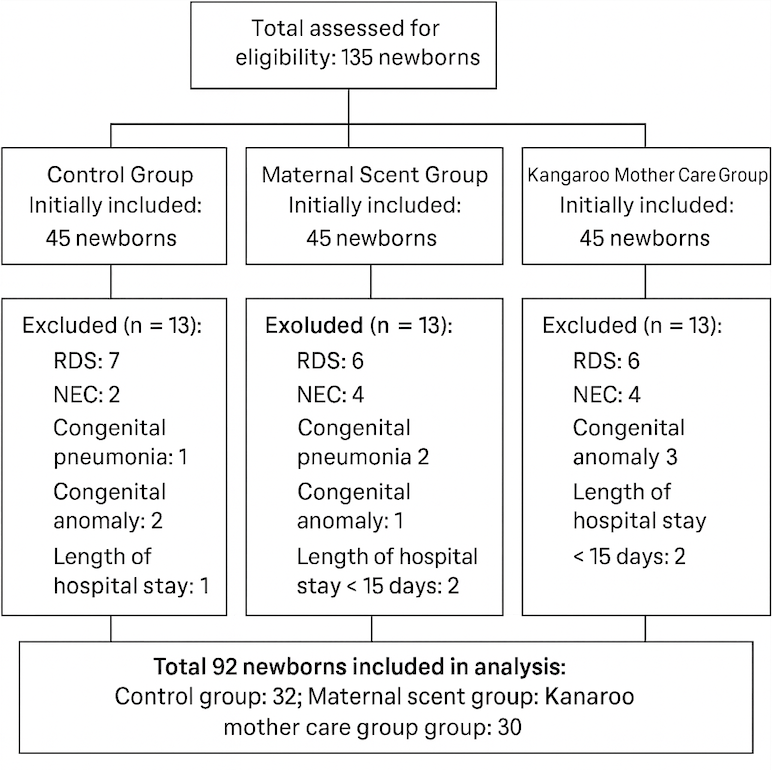
Figure 1. CONSORT flow diagram. RDS: respiratory distress syndrome; NEC: necrotizing enterocolitis.
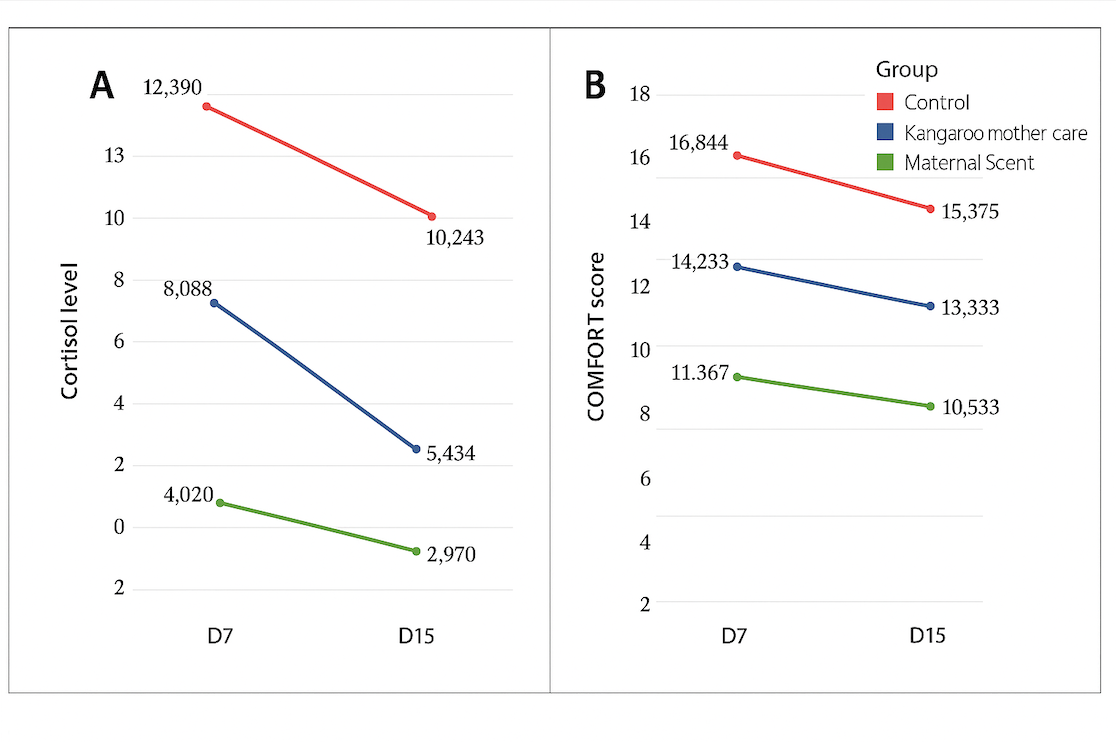
Figure 2. Changes in mean cortisol levels and COMFORT scores of preterm infants on Days 7 and 15. (A) Cortisol level, (B) COMFORT score.
Tables
Table 1. General characteristics of preterm infants and their mothers
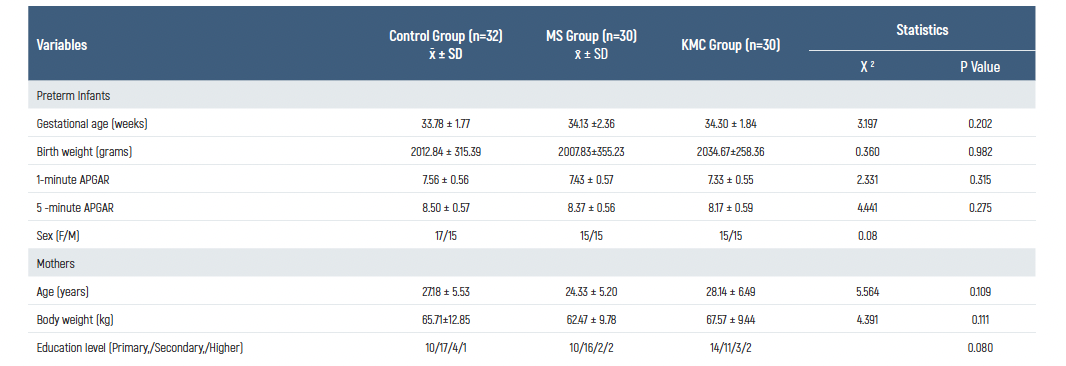
x̄= mean; SD= standard deviation.
Table 2. Analysis of vital signs, cortisol levels, and COMFORT scores at 7 and 15 days of the preterm infants in the control group
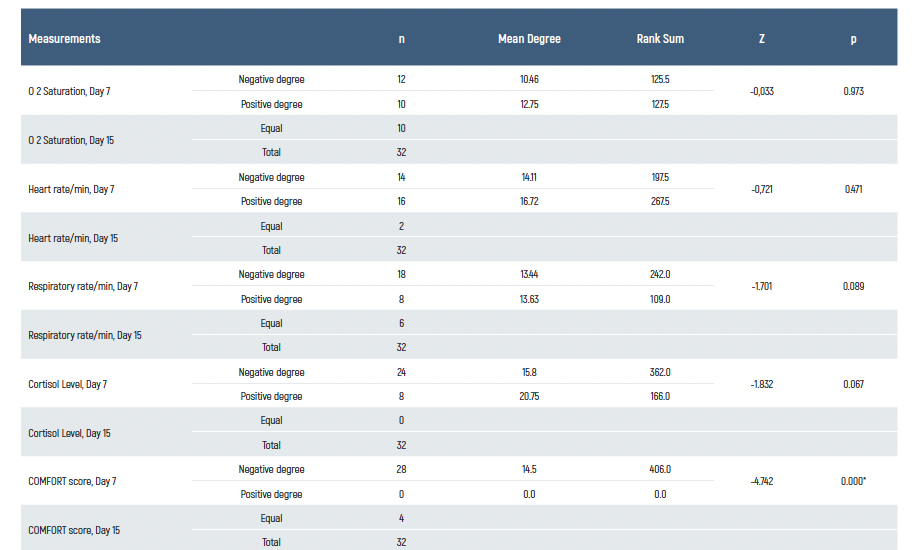
*Statistically significant (<0.05). Wilcoxon Signed-Rank test.
Table 3. Analysis of vital signs, cortisol levels, and COMFORT scores at 7 and 15 days of the preterm infants in the maternal scent group
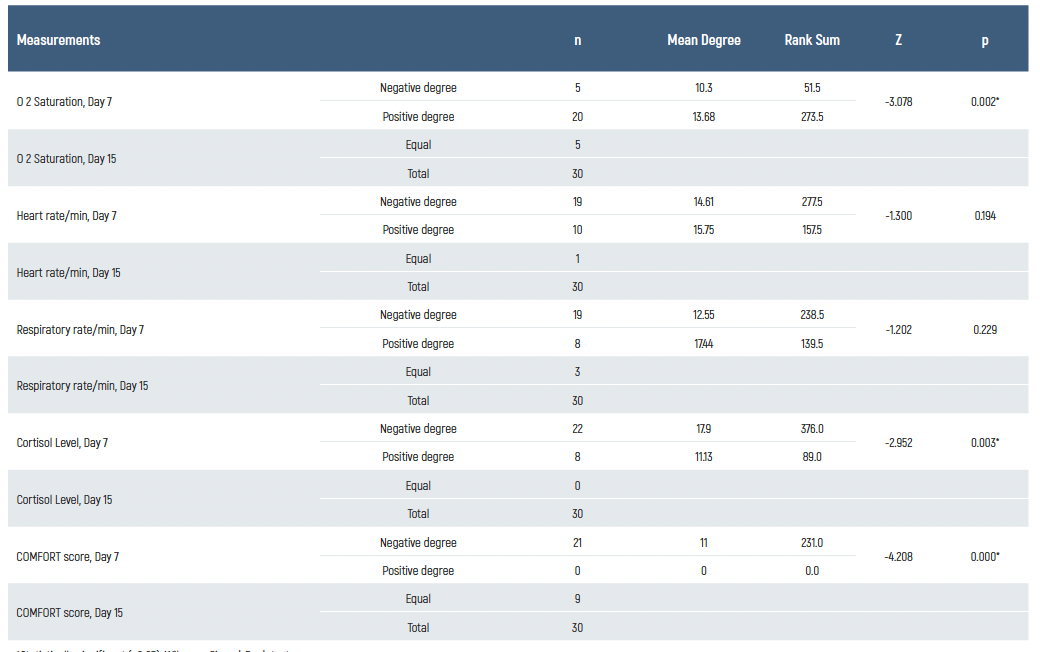
*Statistically significant (<0.05). Wilcoxon Signed-Rank test.
Limitations
This study has some limitations. First, it was conducted in a single neonatal intensive care unit (NICU), which may limit the generalizability of the findings to other healthcare settings with different protocols and patient populations. Second, although maternal scent exposure was standardized using the mother’s worn undershirt, variations in maternal diet, hygiene practices, and genetic factors could have influenced the effectiveness of olfactory stimulation. Another limitation is the potential variability in maternal scent composition due to individual differences in diet, hygiene, and genetic factors, which were not controlled in this study
Conclusion
The findings of this study emphasize the importance of maternal scent in preventing and reducing stress in preterm infants, drawing attention to its role as a non-pharmacological intervention in NICU care. Given the significant reduction in stress markers observed with maternal scent exposure, these results highlight the need to incorporate maternal scent as a standard alternative when Kangaroo Mother Care (KMC) is not feasible, particularly in NICU settings with visitation restrictions. NICU staff must recognize that situations like pandemic restrictions, maternal health conditions, or logistical challenges may hinder direct maternal-infant contact. In such cases, providing maternal scent as part of routine NICU care can serve as a simple yet effective strategy to mitigate the physiological stress responses of preterm infants.
Furthermore, the observed increase in serum cortisol levels in infants experiencing maternal separation underscores the critical need for promoting early and consistent mother-infant contact. NICU personnel should prioritize KMC as the gold standard intervention for stress reduction and physiological stabilization in preterm infants, ensuring its implementation whenever possible. Future research should explore the integration of maternal scent exposure with KMC to determine whether their combined use yields additional benefits for neonatal outcomes.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Altimier L, Phillips R. The neonatal integrative developmental care model: Advanced clinical applications of the seven core measures for neuroprotective family-centered developmental care. Newborn Infant Nurs Rev. . 2016;16(4):230-44.
-
Wiley F, Raphael R, Ghanouni P. NICU positioning strategies to reduce stress in preterm infants: a scoping review. Early Child Dev Care.. 2021;191(15):2333-50.
-
Pados BF, Hess F. Systematic review of the effects of skin-to-skin care on short-term physiologic stress outcomes in preterm infants in the neonatal intensive care unit. Adv Neonatal Care. . 2020;20(1):48-58.
-
Lübke KT, Pause BM. Always follow your nose: The functional significance of social chemosignals in human reproduction and survival. Horm Behav. 2015;68134-44.
-
Çamur Z, Erdoğan Ç. The Effects of Breastfeeding and Breast Milk Taste or Smell on Mitigating Painful Procedures in Newborns: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Breastfeed Med. 2022;17(10):793-804.
-
Kim J, Choi SJ. Effect of Olfactory Stimulation with Breast Milk on Pain Responses to Heel Stick in Premature Infants: A Randomized Controlled Trial. Breastfeed Med. 2022;17(7):605-10.
-
Karakoç A, Kübra G, Celikel T. The Effects of Cord Clamping Time and Early Skin-to-Skin Contact on Maternal Birth Satisfaction in Term Infants. Clin Exp Health Sci.. 2020;10(4):355-61.
-
Alemdar DK, Tüfekçi FG. Prematüre Bebek Konfor Ölçeği’nin Türkçe Geçerlilik ve Güvenilirliği. Hemşirelikte Eğitim ve Araştırma. 2015;12(2):142-8.
-
Caljouw MA, Kloos MA, Olivier MY, Heemskerk IW, Pison WC, Stigter GD, et al. Measurement of pain in premature infants with a gestational age between 28 to 37 weeks: validation of the adapted COMFORT scale. J Neonatal Nurs. 2007;13(1):13-8.
-
Forde D, Fang ML, Miaskowski C. A Systematic Review of the Effects of Skin-to-Skin Contact on Biomarkers of Stress in Preterm Infants and Parents. Adv Neonatal Care. 2022;22(3):223.
-
Bergman NJ. Birth practices: Maternal-neonate separation as a source of toxic stress. Birth Defects Res. 2019;111(15):1087-109.
-
Loman MM, Gunnar MR. Early experience and the development of stress reactivity and regulation in children. Neurosci Biobehav Rev. 2010;34(6):867-76.
-
Boundy EO, Dastjerdi R, Spiegelman D, Fawzi WW, Missmer SA, Lieberman E, et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. 2016;137(1):1-9.
-
Campbell-Yeo M, Johnston CC, Benoit B, Disher T, Caddell K, Vincer M, et al. Sustained efficacy of kangaroo care for repeated painful procedures over neonatal intensive care unit hospitalization: a single-blind randomized controlled trial. Pain. 2019;160(11):2580-8.
-
M Ludington-Hoe S. Evidence-based review of physiologic effects of kangaroo care. Curr Womens Health Rev. 2011;7(3):243-53.
-
Sen E, Manav G. Effect of Kangaroo care and oral sucrose on pain in premature infants: A randomized controlled trial. Pain Manag Nurs. 2020;21(6):556-64.
-
Wang F, Zhang Q, Ni ZH, Lv HT. Effects of kangaroo care on pain relief in premature infants during painful procedures: A meta-analysis. J Spec Pediatr Nurs. 2022;27(4):1-9.
-
Zhang S, Su F, Li J, Chen W. The analgesic effects of maternal milk odor on newborns: a meta-analysis. Breastfeed Med. 2018;13(5):327-34.
-
De Clifford-Faugere G, Lavallee A, Khadra C, Ballard A, Colson S, Aita M. Systematic review and meta-analysis of olfactive stimulation interventions to manage procedural pain in preterm and full-term neonates. Int J Nurs Stud. 2020;110(1):103697.
-
Maayan-Metzger A, Kedem-Friedrich P, Bransburg Zabary S, Morag I, Hemi R, Kanety H, et al. The impact of preterm infants’ continuous exposure to breast milk odor on stress parameters: A pilot study. Breastfeed Med. 2018;13(3):211-4.
-
Souza-Vogler SRd, Lima GMdS. The effect of kangaroo care on modulate chronic stress response in preterm infants and mothers. Stress. 2021;1(2):1-11.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Sanko University (Date: 2020-01-15, No: 2020/15)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Alev Sivasli, Zerrin Çiğdem, Ercan Sivasli. Maternal absence in the neonatal intensive care unit during the pandemic: Can maternal scent mimic kangaroo mother care for preterm ınfants? Eu Clin Anal Med 2025;13(2):23-28
Publication History
- Received:
- February 6, 2025
- Accepted:
- April 2, 2025
- Published Online:
- April 16, 2025
- Printed:
- May 1, 2025
