Our results of the single anterior portal Bankart repair in patients developing anterior shoulder instability with trauma
Bankart repair in anterior shoulder instability
Authors
Abstract
Aim Arthroscopic Bankart repair, a standard treatment for anterior glenoid labrum injuries caused by traumatic shoulder dislocation, is typically performed using two or more portals. This study presents outcomes of a single anterior portal technique.
Material and Methods Between 2014 and 2018, 53 patients (49 males, 4 females) with 54 shoulders underwent arthroscopic Bankart repair by a single surgeon. Patients with bone defects exceeding 25% glenoid bone loss or non-traumatic dislocations, including habitual and atraumatic instability, were excluded. Preoperatively, all patients underwent instability tests, X-rays, and MRI. Surgery was performed under general anesthesia in the lateral decubitus position, using a posterior portal for glenoid access. After four weeks of immobilization, all patients followed a rehabilitation program.
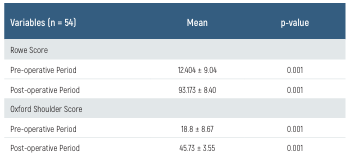
Results The mean patient age was 28 years (range: 16–66), with a mean follow-up of 26 months (range: 9–60). The lesion was on the right side in 34 patients and left side in 20 patients. The mean time from first dislocation to surgery was 45.8 months (range: 1–288), and the mean number of preoperative dislocations was 17.5 (range: 1–60). The mean number of anchors used was 3 (range: 1–5), and the average surgery duration was 44.6 minutes (range: 32–70). Postoperatively, three patients had a positive apprehension test, but no recurrent dislocations or reductions were required. The mean Rowe score improved from 12.4 ± 9.04 to 93.1 ± 8.40 (p=0.001), and the mean Oxford score from 18.8 ± 8.67 to 45.7 ± 3.55 (p=0.001).
Discussion The single-portal technique is a cost-effective, less invasive alternative with a shorter learning curve compared to multi-portal techniques. Studies have reported that multi-portal approaches, while widely used, may result in increased surgical time and morbidity. In contrast, the single-portal method minimizes soft tissue disruption and offers comparable clinical outcomes with a lower complication rate, making it a favorable option for surgeons and patients.
Keywords
Introduction
The glenohumeral joint is the most mobile in the human body, providing a wide range of motion essential for daily activities. However, this mobility comes at the cost of stability, particularly when exposed to trauma. Shoulder instability, particularly anterior shoulder instability, is the most common form of recurrent joint instability, accounting for approximately 50% of all dislocations. The recurrence rate of shoulder instability is notably high, especially in younger, more active populations 1,2.
The stability of the shoulder joint is maintained by both static and dynamic structures. Key stabilizers include the surrounding muscles, such as the deltoid and rotator cuff muscles, as well as the extracapsular ligaments. These ligaments perform crucial roles in preventing both superior-inferior translation and maintaining anterior stability. Among these, the inferior glenohumeral ligament is regarded as the primary static stabilizer of the shoulder joint 3,4,5.
Laxity is a natural feature of the shoulder joint; however, when it becomes excessive to the point of clinical concern, it is classified as instability. The primary cause of shoulder instability is trauma, which is responsible for about 95% of all shoulder dislocations. Of these, 98% involve anterior dislocation, while only 2% result in posterior dislocation. Traumatic anterior glenohumeral instability occurs in ~1.7% of the general population. Following conservative treatment, the risk of recurrence is particularly high in patients under 20 years old, with rates exceeding 90%, whereas in patients over 40 years old, the recurrence rate drops below 10% 5,6.
A common sequela of traumatic anterior shoulder dislocation is the Bankart lesion, which involves the detachment of the glenoid labrum from the anterior-inferior aspect of the glenoid rim. This detachment leads to compromised stability, as the labrum and associated capsuloligamentous structures contribute to the passive stabilization of the glenohumeral joint by deepening the glenoid cavity and serving as an attachment site for the inferior glenohumeral ligament 7.
The gold standard treatment for Bankart lesions is now arthroscopic repair, 8. While successful outcomes have been reported with the use of two or more anterior portals for arthroscopic Bankart repair, there is growing interest in minimally invasive techniques that limit surgical morbidity. Conventional two-portal techniques, while widely adopted, may be associated with increased surgical time, potential iatrogenic cartilage damage, and greater postoperative pain due to the need for additional soft tissue dissection, 9. Additionally, a steeper learning curve for novice surgeons has been noted with the conventional approach. In contrast, the single anterior portal technique has been proposed as a viable alternative, reducing the number of incisions while maintaining surgical effectiveness. Studies suggest that this approach results in lower postoperative pain scores, shorter operative time, and reduced costs compared to multi-portal techniques 10,11. In this study, we present our results using a single anterior portal for arthroscopic Bankart repair in patients with traumatic anterior shoulder instability. We believe that the single anterior portal technique offers a less invasive, safe, and effective approach to treating Bankart lesions, with promising outcomes in terms of stability and functional recovery.
Materials and Methods
Study Design, Settings, and Sample
This retrospective study was conducted by reviewing patients who underwent arthroscopic modified Bankart surgery for recurrent anterior shoulder dislocation due to trauma at the Gaziantep University Orthopedics and Traumatology Clinic between 2014 and 2018. All patients included in the study were treated by a single experienced surgeon using a single anterior portal approach for arthroscopic stabilization surgery. The patients’ demographic information, such as age, gender, side of the injury, mechanism of the first dislocation, number of dislocations, method of reduction after dislocations, presence of additional diseases, and the time interval between the first dislocation and the surgery were evaluated. Preoperative physical examination findings, including the apprehension test, O’Brien test, Jerk test, Sulcus sign, and acromion types, were recorded. Additionally, data on the surgery duration, number of anchors used, presence of Hill- Sachs lesion, rotator cuff status, and pre- and postoperative Oxford and Rowe scores were documented. A total of 87 patients who underwent arthroscopic modified Bankart surgery for recurrent anterior shoulder dislocation were included in the study. Patients with recurrent anterior shoulder dislocations who did not respond to conservative treatment, those with symptoms of anterior shoulder instability, and patients with less than 25% glenoid bone loss identified during arthroscopy were included in the study. Patients with a Hill-Sachs defect larger than 20%, atraumatic or habitual dislocations, those who had undergone multiple modified arthroscopic Bankart procedures, patients who did not attend regular follow-ups, and those who did not adhere to postoperative exercise protocols were excluded from the study. Of the 87 operated patients, 53 met the inclusion criteria. One patient had dislocations in both shoulders at different times, resulting in a total of 54 shoulder cases being included in the study.
Surgical Procedure
All patients were positioned in the lateral decubitus position, and a posterior portal was first established after proper preparation. Before the anterior portal was created, a spinal needle was used to determine the optimal angle and position for accessing the glenoid labrum and anteroinferior capsule. Guided by the needle, a single anterior portal was then opened. Postoperatively, all patients were placed in an internal rotation shoulder sling for 4 weeks. Passive exercises were initiated immediately after surgery, while active exercises began at week 4. Strengthening exercises were introduced between weeks 8 and 12, and patients were allowed to return to sports activities after the 6th month. Follow-ups were conducted at 3 weeks, 6 weeks, 3 months, 6 months, and 12 months post-surgery, with annual check-ups thereafter. During follow-ups, shoulder range of motion and instability tests were assessed.
Statistical analysis
All analyses were performed using the SPSS Windows version 25.0 (IBM, NY, USA), and a p-value of <0.05 was considered statistically significant. The normality of the distribution of numerical variables was assessed using the Shapiro-Wilk test. The Mann-Whitney U test was used to compare non-normally distributed variables between two independent groups, while the Wilcoxon test was applied for the comparison of non-normally distributed dependent variables. Relationships between non-normally distributed numerical variables were evaluated using the Spearman rank correlation coefficient. Parametric tests were applied for normally distributed data, while non-parametric tests were used for non-normally distributed variables.
Ethics approval
This study was approved by the Ethics Committee of the Gaziantep University (Date: 2018-01-15, No: 2018/01).
Written informed consent was obtained from the parents of the infants after explaining them the study purpose, scope and procedures.
Results
A total of 54 shoulders from 53 patients, including one patient with bilateral involvement, were included in the study, all treated with arthroscopic surgery using a single anterior portal. The lesion was observed in the dominant shoulder in 28 patients and the non-dominant shoulder in 26 patients. The average time from the first dislocation to the surgical treatment in patients was 45.8 months (range 1-288 months). At the time of presentation, the average number of dislocations was 17.5 (range 1-60), and the average number of anchors used during surgery was 3 (range 1-5). The Hill-Sachs lesion was present at a high rate of 92.6%. Among the patients, 38 (70.4%) had type 1 acromion, 13 (24.1%)
had type 2 acromion, and 3 (5.6%) had type 3 acromion. The average surgical duration was 44.6 minutes (range 32-70 minutes). The general descriptive characteristics and demographic data of the patients are shown in Table 1 and Table 2.
In the postoperative period, the apprehension test was found to be positive in 3 patients, but no recurrent dislocation was detected during their follow-up, and none required additional surgical intervention. The preoperative average Rowe score was 12.4 ± 9.04, while the postoperative average Rowe score increased significantly to 93.17 ± 8.40 (p = 0.001). Similarly, the preoperative average Oxford Shoulder score was 18.8 ± 8.67, which increased to 45.73 ± 3.55 in the final postoperative follow-up, indicating a significant improvement (p = 0.001) (Table 3). One patient experienced redislocation 2 years after surgery while attempting a spike in volleyball, and another patient experienced redislocation 3 months after surgery due to lying on the shoulder during sleep. No other complications were reported.
A correlation analysis was conducted to investigate the relationship between the number of dislocations and the preoperative Rowe and Oxford scores. There was a statistically significant positive correlation between the number of dislocations and the preoperative Oxford score (r = 0.341, p = 0.013). However, no significant correlation was found between the number of dislocations and the preoperative Rowe score (r = 0.251, p = 0.068). Additionally, a strong positive correlation was observed between the preoperative Rowe score and the preoperative Oxford score (r = 0.555, p <0.001), indicating that as the preoperative Rowe score increases, the preoperative Oxford score also increases. The number of patients with a SLAP lesion in addition to a Bankart lesion was 5. Due to the small number of patients with SLAP lesions, the Rowe and Oxford scores were not significantly different compared to those with only Bankart lesions.
In 11 of the 53 patients (20.7%), the first dislocation occurred during military service or mandatory conscription.
Discussion
In this study, we evaluated the outcomes of patients who underwent arthroscopic Bankart repair using a single anterior portal for recurrent traumatic shoulder dislocations. Our results demonstrate that this technique is both effective and minimally invasive, providing excellent clinical outcomes. The significant improvement in both Rowe and Oxford scores postoperatively highlight the success of this approach in restoring shoulder stability and function. Compared to traditional methods involving multiple portals, the single anterior portal technique offers the advantage of reduced invasiveness without compromising surgical efficacy.
Several studies have compared the single and double anterior portal techniques in terms of surgical time, complications, post-operative pain, and recurrence rates. The single anterior portal technique has been associated with significantly shorter operative time due to reduced portal placement and instrument exchange requirements, 8,12,13,14. Cicek et al. reported that the single-portal approach resulted in an average surgical duration of 35 minutes, compared to 53.3 minutes for the double-portal technique, 12. Similarly, our study found an average surgical time of 44.6 minutes, supporting the efficiency of this approach. Additionally, studies have suggested that the single anterior portal technique may result in less post-operative pain and faster recovery due to reduced soft tissue trauma, 13,14. Recurrence rates appear to be comparable between the two techniques, reinforcing the clinical viability of the single-portal method, 15.
One of the major challenges associated with the single-portal technique is anchor placement, particularly at the 5 o’clock position. Reda et al. suggested that creating a posterolateral portal might provide a better bumper effect at the 6 o’clock position, 14. In our study, the greatest difficulty was encountered when placing the suture anchor at the 5 o’clock position, indicating that additional technical expertise is required for optimal anchor positioning.
The shoulder joint is the most commonly dislocated large joint in the body. Although shoulder dislocations are particularly common in young adults, there is limited knowledge about the epidemiology of shoulder instability 6,16. Various reports have been published on the incidence of traumatic shoulder dislocations in the general population. Hovelius et al. found the incidence of shoulder dislocation in people aged 18-70 to be at least 1.7%, with it being three times more common in men, 17. In our study, the incidence was found to be 94% in men and 6% in women.
Shoulder instability is more frequently observed in young, athletic individuals and military personnel, with an incidence rate of 2.8% 13. In our study, 20.7% of patients experienced their first dislocation while serving as military personnel or during mandatory military service.
The posterolateral aspect of the humeral head should be examined for a possible Hill-Sachs lesion, which is pathognomonic for shoulder instability and is observed in approximately 80% of patients with recurrent anterior dislocations 18,19,20. In the literature, the reported incidence of Hill-Sachs lesions following traumatic anterior instability ranges from 60% to 90% 5,11,21,22. In our study, the incidence of Hill- Sachs lesions was found to be 93%.
Similar to the occurrence of the first dislocation, it is believed that the recurrence of dislocation and the development of anterior instability are more frequently observed on the dominant side due to its higher usage compared to the non-dominant side. However, Lim et al. concluded that traumatic shoulder dislocations induced by sports were equally likely to occur in both the dominant and non-dominant arms, making it difficult to predict future injuries based on hand dominance 16. When making comparisons, it is important to consider whether the instability developed as a result of trauma or not. In our study, which included only patients with trauma-induced anterior instability, 52% of recurrent dislocations were observed on the dominant side, while 48% occurred on the non-dominant side.
In cases of acute traumatic anterior dislocations, after diagnosis and neurological examination, the first line of treatment is closed reduction. The reduction of the shoulder joint should be performed promptly and gently. While reduction in the acute phase can often be achieved without the need for analgesia, brachial plexus block, regional anesthesia, or general anesthesia may sometimes be required 5. In our study, only 5 patients (9.2%) had their initial dislocation reduced in the emergency department of our hospital. Additionally, these patients had an average of 4 dislocations (compared to the overall patient average of 17.5), which is relatively low. When we asked patients whose initial or recurrent dislocations were reduced at other centers, many indicated that, despite visiting a hospital or even being seen by an orthopedist, they were not informed about the possibility of surgery after recurrent dislocations or the potential need for surgery after the initial dislocation if instability recurred. We believe this lack of information may be one of the reasons for the higher number of dislocations and the prolonged time between the first dislocation and surgery.
Although arthroscopic Bankart repair is commonly performed using two or more portals, it is also possible to carry out the procedure with a single anterior portal. The single anterior portal technique has several advantages over the double anterior portal approach, including lower cost, reduced postoperative pain, and a shorter learning curve. In a study by Cicek et al., involving 91 patients, a comparison was made between the single anterior portal and double portal techniques for traumatic anterior shoulder dislocations. The study found that the single anterior portal resulted in less postoperative pain, lower costs, and a shorter learning curve, 12. Additionally, the average surgery duration was 35 minutes for the single portal technique and 53.3 minutes for the double portal technique. In our study, while we did not assess postoperative pain or cost, the average surgery duration was 44.6 minutes, which aligns with previous findings.
Our study also found a statistically significant improvement in both Rowe and Oxford scores postoperatively. A study by Kalkar et al. involving 22 patients with an average follow-up of 30 months reported a postoperative Rowe score of 95.5 and an Oxford score of 44.6 13. In comparison, our study found a postoperative Rowe score of 93.1 and an Oxford score of 45.7, demonstrating similar clinical outcomes. Additionally, we identified a weak but significant correlation between the number of dislocations and the preoperative Oxford score, with the preoperative Oxford score increasing as the number of dislocations increased.
Future studies with larger sample sizes and long-term follow-up are needed to further validate the effectiveness and safety of the single anterior portal technique in comparison with conventional multi-portal approaches.
Tables
Table 1
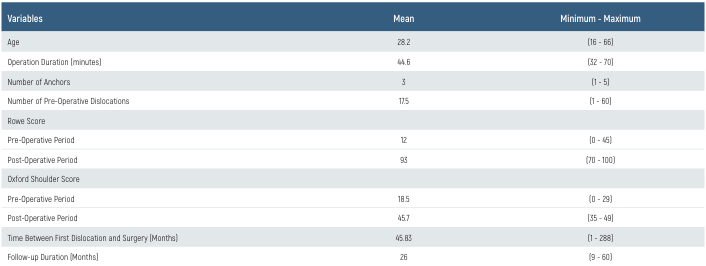
Table 2
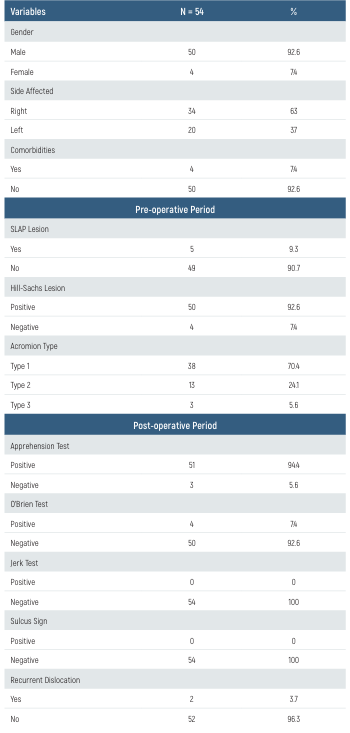
Table 3
Limitations
The limitations of this study include a relatively small sample size, which may restrict the generalizability of the results. Additionally, since the study was conducted at a single center within a specific setting, the findings may not be fully applicable to other healthcare institutions or broader patient populations. Moreover, while the single-portal technique has demonstrated advantages such as reduced invasiveness and cost-effectiveness, it also presents technical challenges, including a steeper learning curve and difficulties in anchor placement at certain positions. Future multicenter studies with larger cohorts are needed to further validate the efficacy and reproducibility of this technique.
Conclusion
Although the use of two anterior portals has become a standard technique in arthroscopic instability surgery, it does come with certain limitations. For instance, if proper planning is not executed, or in smaller patients, it may not always be possible to effectively place and utilize two separate cannulas throughout the surgery. In single-portal surgery, however, these limitations are avoided. In modern treatment options, less invasive techniques are becoming increasingly preferred. The reported advantages of arthroscopic surgery for shoulder instability include shorter hospital stays, less postoperative pain and movement loss, shorter surgery times, lower morbidity, better cosmetic outcomes, and fewer complications. The disadvantages of arthroscopic surgery include a longer learning curve and the need for specialized equipment and tools.
In conclusion, the single-portal technique for the arthroscopic repair of Bankart lesions resulting from traumatic anterior shoulder dislocation is not only a more cost-effective and less invasive option, but it also requires fewer instruments and has a shorter learning curve compared to the double-portal technique, making it a favorable choice.
Data Availability
The data supporting the findings of this article are available from the corresponding author upon reasonable request, due to privacy and ethical restrictions. The corresponding author has committed to share the de-identified data with qualified researchers after confirmation of the necessary ethical or institutional approvals. Requests for data access should be directed to bmp.eqco@gmail.com
References
-
Magnuson JA, Wolf BR, Cronin KJ, Jacobs CA, Ortiz SF, Kuhn JE, et al. Surgical outcomes in the Frequency, Etiology, Direction, and Severity (FEDS) classification system for shoulder instability. J Shoulder Elbow Surg. 2020;29(4):784-93.
-
Stolwijk PJ, Verweij LPE, Kerkhoffs G, van Deurzen DFP, Priester-Vink S, Sierevelt IN, et al. Patient-Reported Outcome Measures Show No Relevant Change Between 1-Year and 2-Year Follow-Up After Treatment for Anterior Shoulder Instability: A Systematic Review. Arthroscopy. 2024(9):1-7.
-
Gao R, Fleet CT, Jin W, Johnson JA, Faber KJ, Athwal GS. The Kouvalchouk procedure vs. distal tibial allograft for treatment of posterior shoulder instability: the deltoid “hammock” effect exists. J Shoulder Elbow Surg. 2024;33(10):537-46.
-
Yi M, Yang F, An J, Huang F. Effect of glenohumeral ligaments on posterior shoulder stabilization: A biomechanical study. Am J Transl Res. 2023;15(3):1953-63.
-
Apostolakos JM, Wright-Chisem J, Gulotta LV, Taylor SA, Dines JS. Anterior glenohumeral instability: Current review with technical pearls and pitfalls of arthroscopic soft-tissue stabilization. World J Orthop. 2021;12(1):1-13.
-
Trojan JD, Meyer LE, Edgar CM, Brown SM, Mulcahey MK. Epidemiology of Shoulder Instability Injuries in Collision Collegiate Sports From 2009 to 2014. Arthroscopy. 2020;36(1):36-43.
-
Gowd AK, Waterman BR. The Arthroscopic Bankart Repair: State of the Art in 2020: Decision-making and Operative Technique. Sports Med Arthrosc Rev. 2020;28(4):25-34.
-
Woodmass JM, McRae S, Lapner P, Kamikovski I, Jong B, Old J, et al. Arthroscopic Bankart Repair With Remplissage in Anterior Shoulder Instability Results in Fewer Redislocations Than Bankart Repair Alone at Medium-term Follow-up of a Randomized Controlled Trial. Am J Sports Med. 2024;52(8):2055-62.
-
Atilgan N, Ipek B, Duman N, Orhan O, Yilmaz M. Can anterolateral thigh flap be a rescuer in lower extremity injuries? Eur Rev Med Pharmacol Sci. 2023;27(15):7005-11.
-
Magnuson JA, Wolf BR, Cronin KJ, Jacobs CA, Ortiz SF, Bishop JY, et al. Sex-related differences in patients undergoing surgery for shoulder instability: a Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Instability cohort study. J Shoulder Elbow Surg. 2019;28(6):1013-21.
-
Friedman LGM, Lafosse L, Garrigues GE. Global Perspectives on Management of Shoulder Instability: Decision Making and Treatment. Orthop Clin North Am. 2020;51(2):241-58.
-
Cicek H, Tuhanioglu U, Ogur HU, Seyfettinoglu F, Ciloglu O, Beyzadeoglu T. Single anterior portal: A better option for arthroscopic treatment of traumatic anterior shoulder instability? Acta Orthop Traumatol Turc. 2017;51(4):298-302.
-
Kalkar I, Esenyel CZ, Saygili MS, Esenyel A, Gurbuz H. The results of Bankart repair without capsular plication in patients with recurrent traumatic anterior shoulder dislocation. J Orthop Surg (Hong Kong). 2017;25(1):1-8.
-
Reda W, Khedr A. Using a Posterolateral Portal to Pass and Tie the Suture of the Inferior Anchor During Arthroscopic Bankart Repair. Arthrosc Tech. 2016;5(6):1467-70.
-
Chin G, Kraeutler MJ, Batiste A, McCarty C, McCarty EC. Management of the in-season athlete with an anterior shoulder dislocation. J Shoulder Elbow Surg.2024;33(12):2780-90.
-
Lim CR, Yap C, Campbell P. Hand dominance in traumatic shoulder dislocations. JSES Open Access. 2018;2(2):137-40.
-
Hovelius L, Rahme H. Primary anterior dislocation of the shoulder: long-term prognosis at the age of 40 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):330-42.
-
Lim JR, Lee HM, Yoon TH, Lee HM, Chun YM. Association Between Excessive Joint Laxity and a Wider Hill-Sachs Lesion in Anterior Shoulder Instability. Am J Sports Med. 2021;49(14):3981-7.
-
Calvo E, Delgado C. Management of off-track Hill-Sachs lesions in anterior glenohumeral instability. J Exp Orthop. 2023;10(1):30-5.
-
Dyrna FGE, Ludwig M, Imhoff AB, Martetschlager F. Off-track Hill-Sachs lesions predispose to recurrence after nonoperative management of first-time anterior shoulder dislocations. Knee Surg Sports Traumatol Arthrosc. 2021;29(7):2289-96.
-
Yu JS, Rink T, Yu SM, Liu K, Carver K, Lather JD, et al. The broken circle method: a novel technique that enhances detection of Hill-Sachs lesions on internal rotation shoulder radiographs. Clin Radiol. 2021;76(2):158-68.
-
Goth AP, Klug A, Gosheger G, Hiort ML, Akgün D, Schneider KN. Traumatic Anterior Shoulder Dislocation: Epidemiology, Diagnosis, and Treatment. Dtsch Arztebl Int. 2025; 122(1):89-95.
Scientific Responsibility Statement
The authors declare that they are responsible for the article’s scientific content including study design, data collection, analysis and interpretation, writing, some of the main line, or all of the preparation and scientific review of the contents and approval of the final version of the article.
Animal and Human Rights Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or compareable ethical standards.
Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethics Declarations
This study was approved by the Ethics Committee of Gaziantep University (Date: 2018-01-15, No: 2018/01)
Additional Information
Publisher’s Note
Bayrakol MP remains neutral with regard to jurisdictional and institutional claims.
Rights and Permissions
About This Article
How to Cite This Article
Ramazan Parildar, Mehmet Yilmaz, Burcin Karsli. Our results of the single anterior portal bankart repair in patients developing anterior shoulder ınstability with trauma. Eu Clin Anal Med 2025;13(2):29-33
Publication History
- Received:
- February 6, 2025
- Accepted:
- April 2, 2025
- Published Online:
- April 22, 2025
- Printed:
- May 1, 2025
